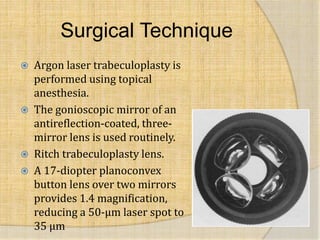
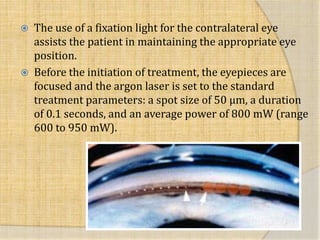
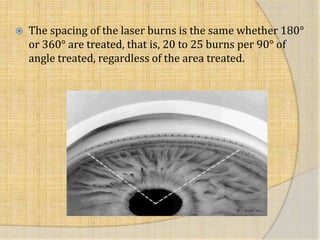
The document discusses the history and techniques of laser trabeculoplasty for treating glaucoma. It was first introduced in 1961 using light energy on the eye's anterior chamber angle. The first successful protocol in 1979 used argon laser and since then different laser types have been developed. Laser trabeculoplasty works by lowering eye pressure through various mechanical and biological mechanisms of the trabecular meshwork. The technique involves using a gonioscopic lens and laser settings are calibrated to the eye to apply spots treating areas of the angle to increase outflow with minimal complications.


![ 1979 Argon Laser [488 nm blue-green, 514 nm
green]
1984 Krypton Laser [red 647.1 nm, yellow 568.2
nm]
1988 Nd:YAG Laser [1064 nm]
1990 Diode Laser [810 nm]
1996 Solid State “ALT” [532 nm]
2001 Frequency Doubled Nd:YAG laser: SLT [532
nm]
2006 Diode MicroPulse Laser: MLT [810 nm]
2008 Titanium:Sapphire Laser [790 nm]](https://image.slidesharecdn.com/argonlaser-150408210726-conversion-gate01/85/Argon-laser-3-320.jpg)