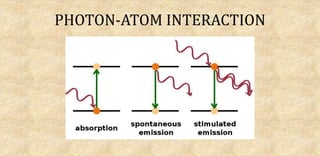
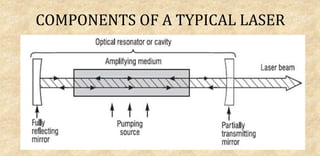
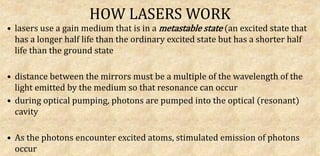
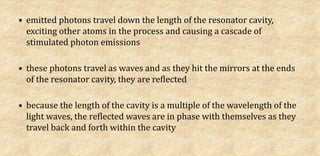
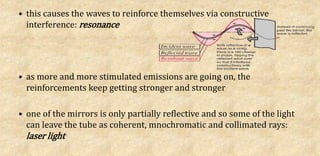
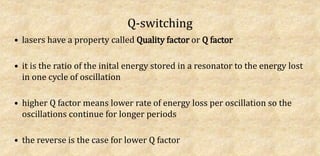
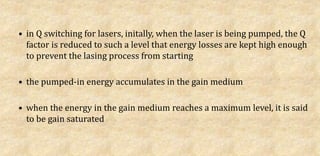
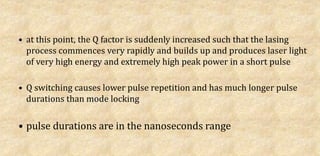
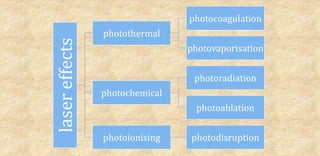
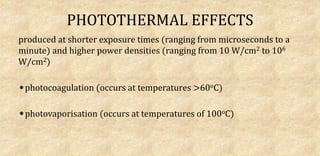
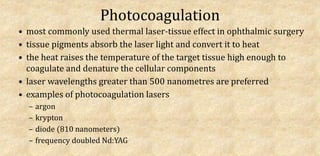
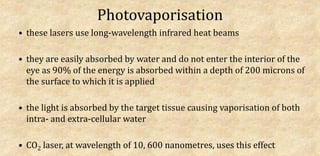
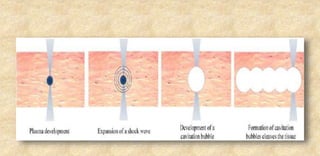
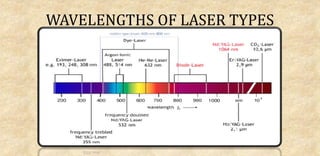
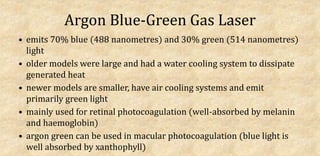
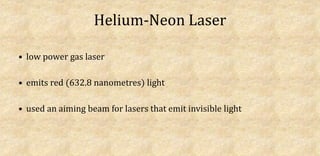
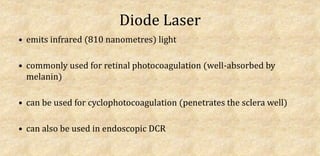
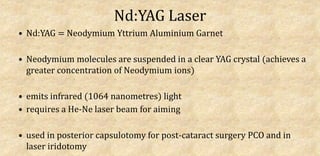
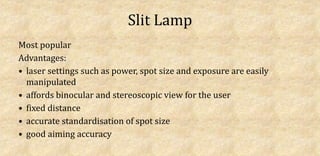
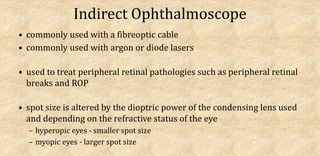
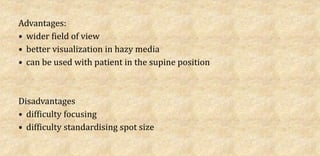
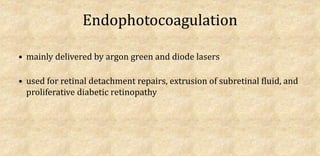
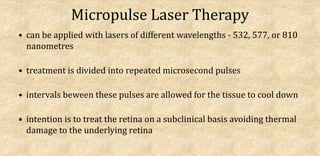
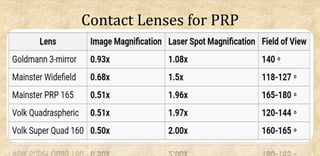
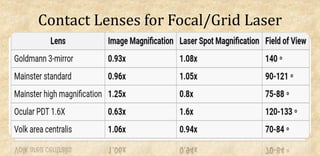
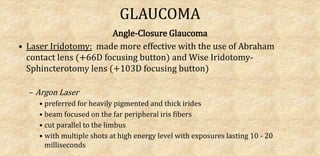
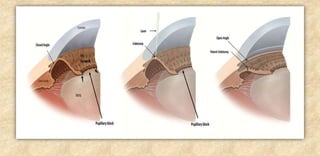
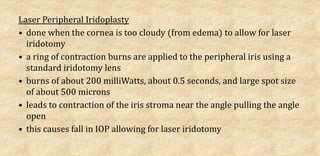
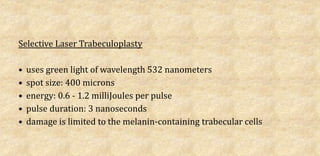
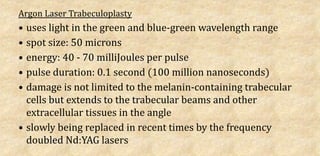
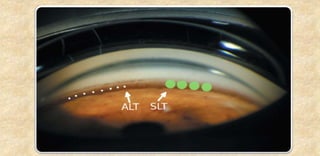
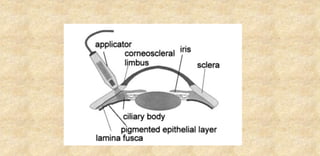
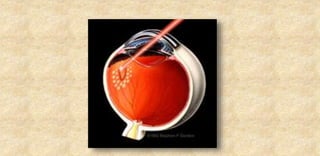
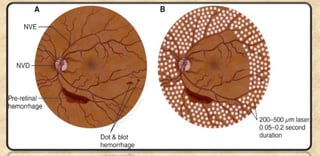
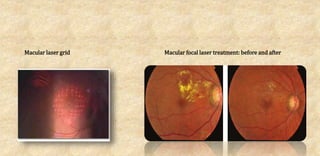
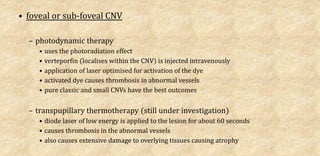
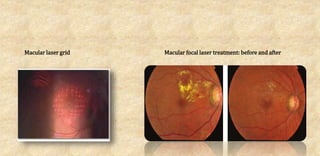
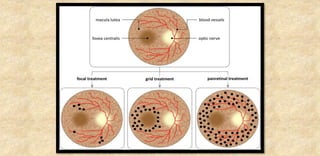
The document provides an extensive overview of laser physics and its applications in ophthalmology, tracing the evolution of lasers from their inception to clinical use. It details various laser types, their operational principles, and effects on ocular tissues, highlighting procedures such as photocoagulation, photovaporization, and laser-assisted surgeries. Additionally, it covers the specific laser delivery systems and technologies utilized in contemporary ophthalmic practices.