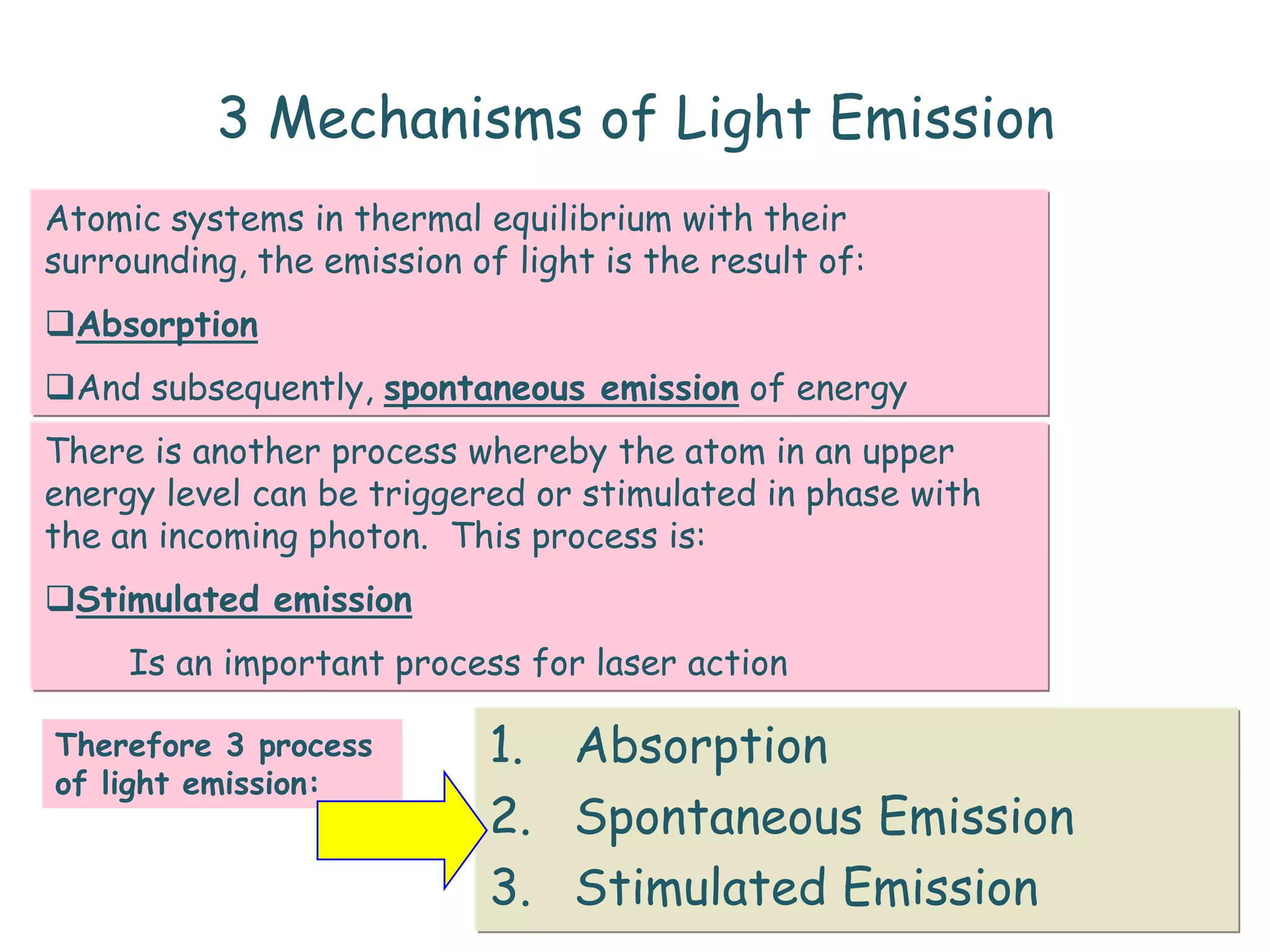
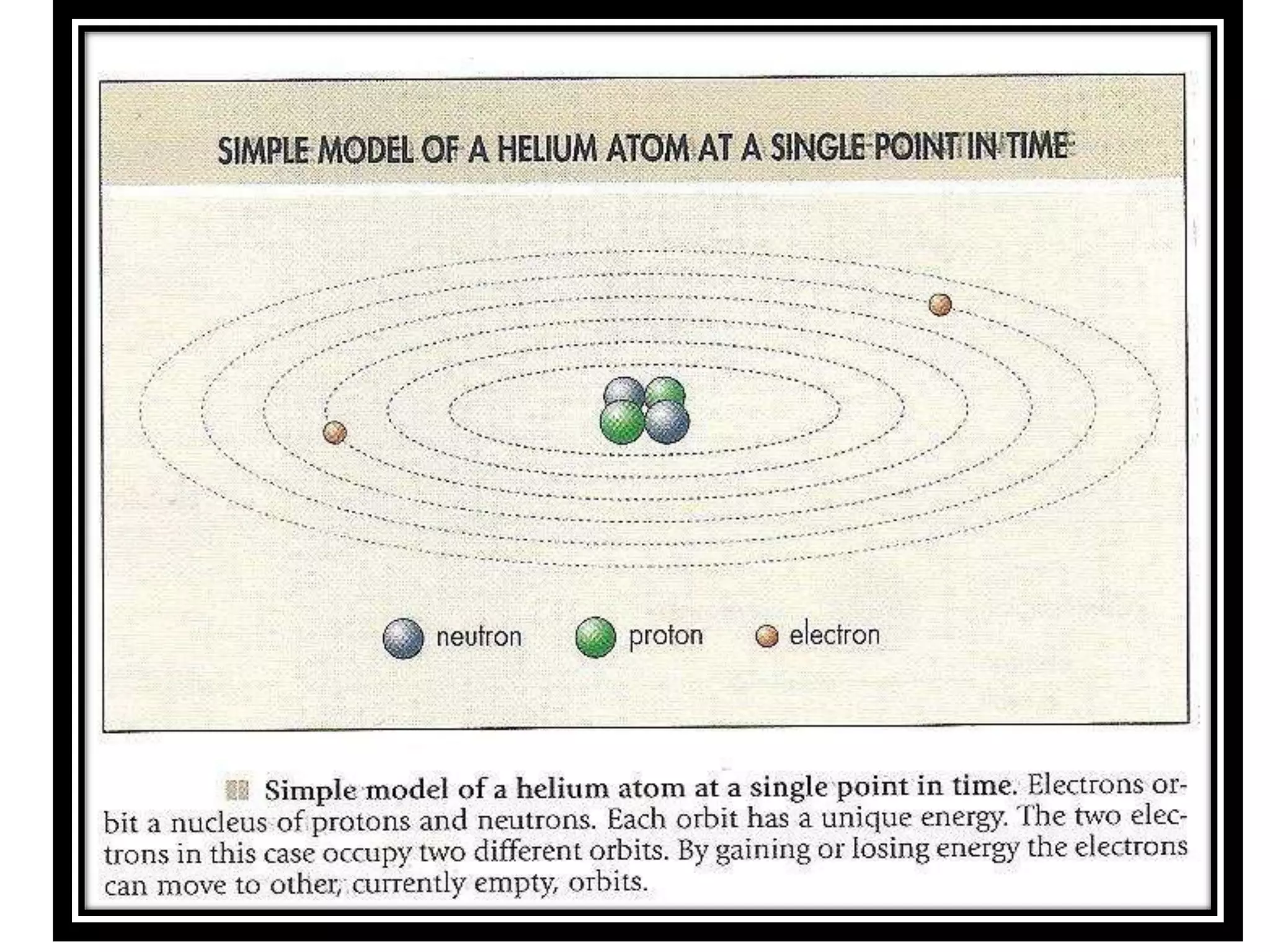
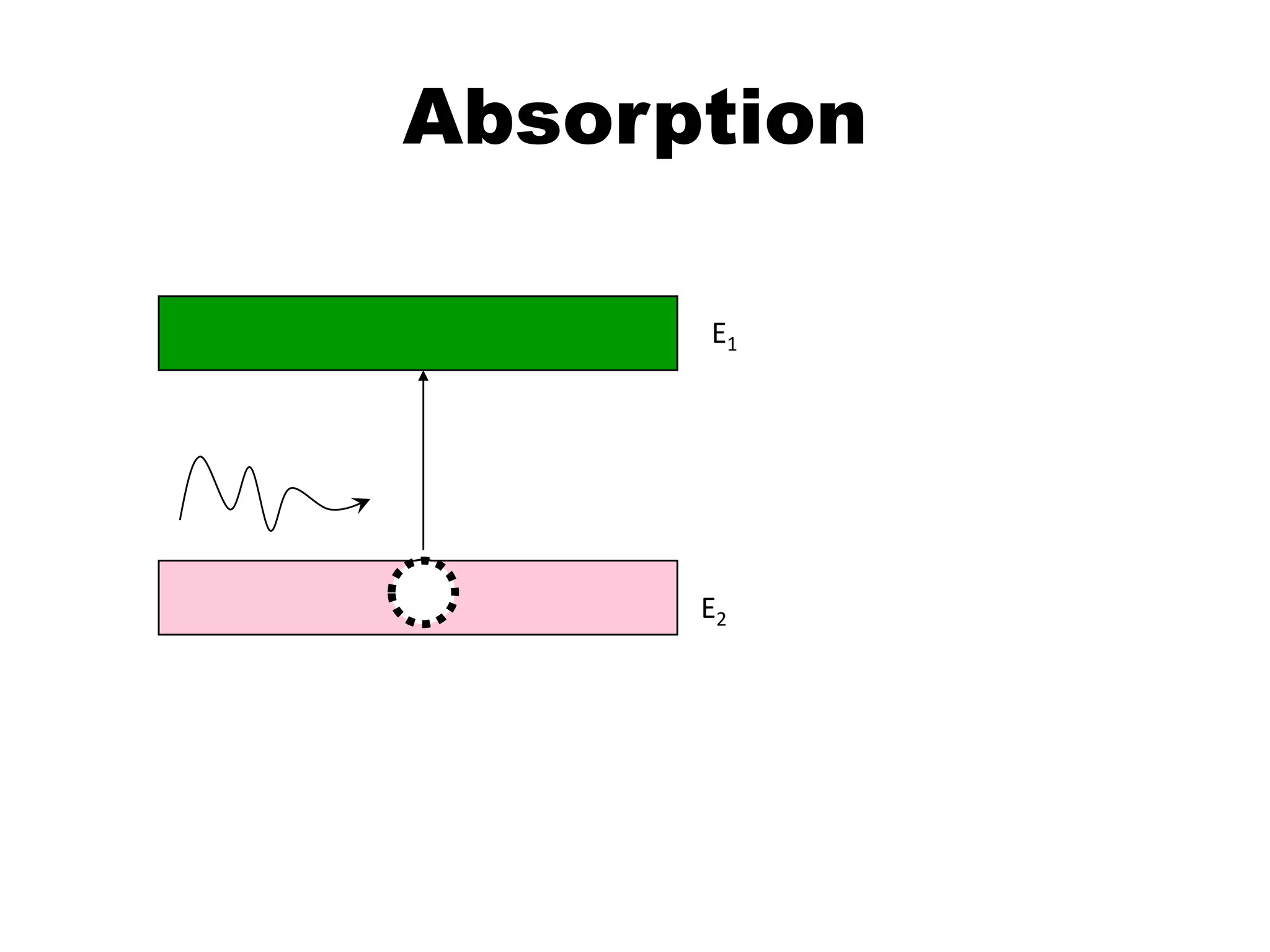
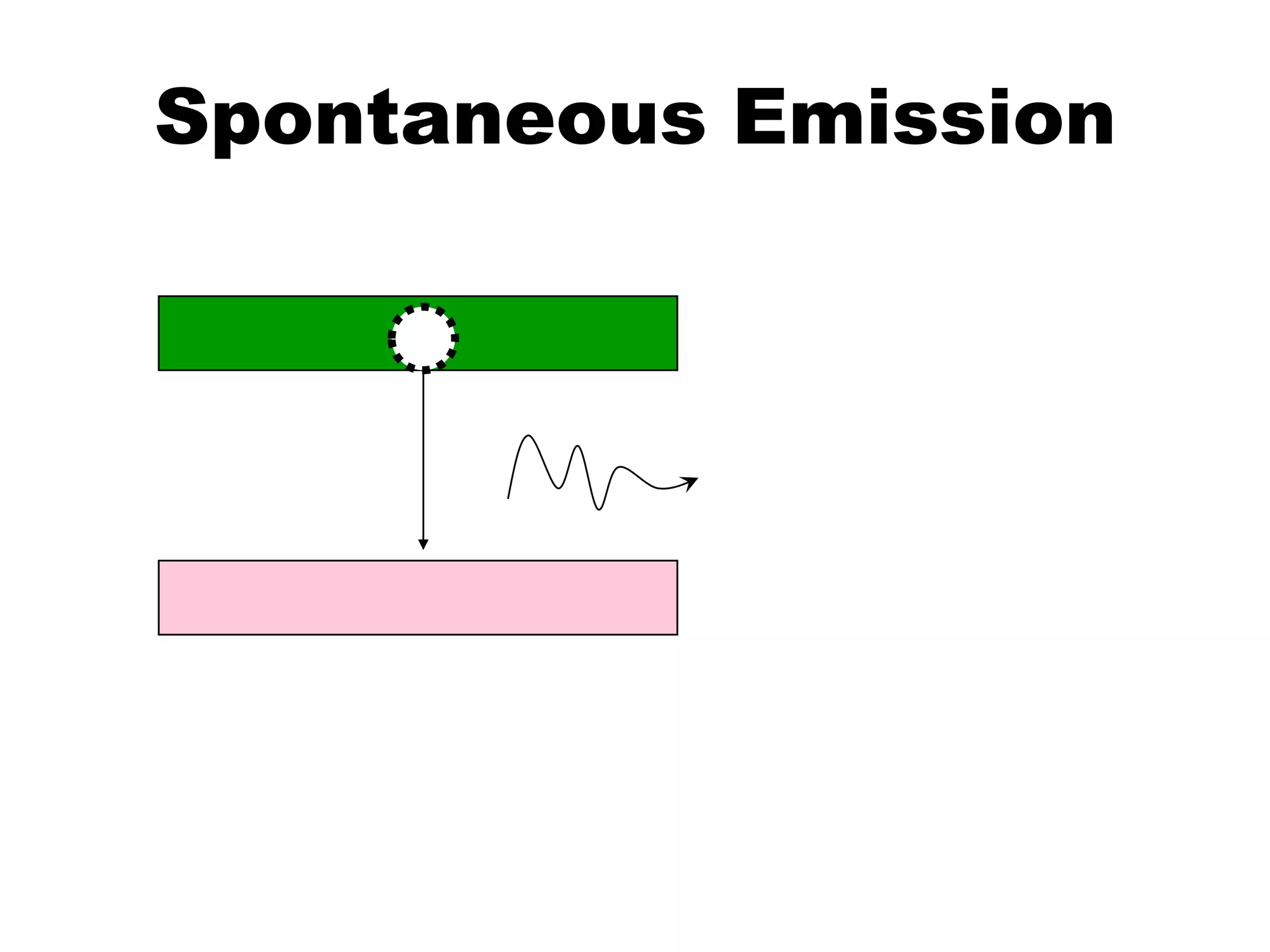
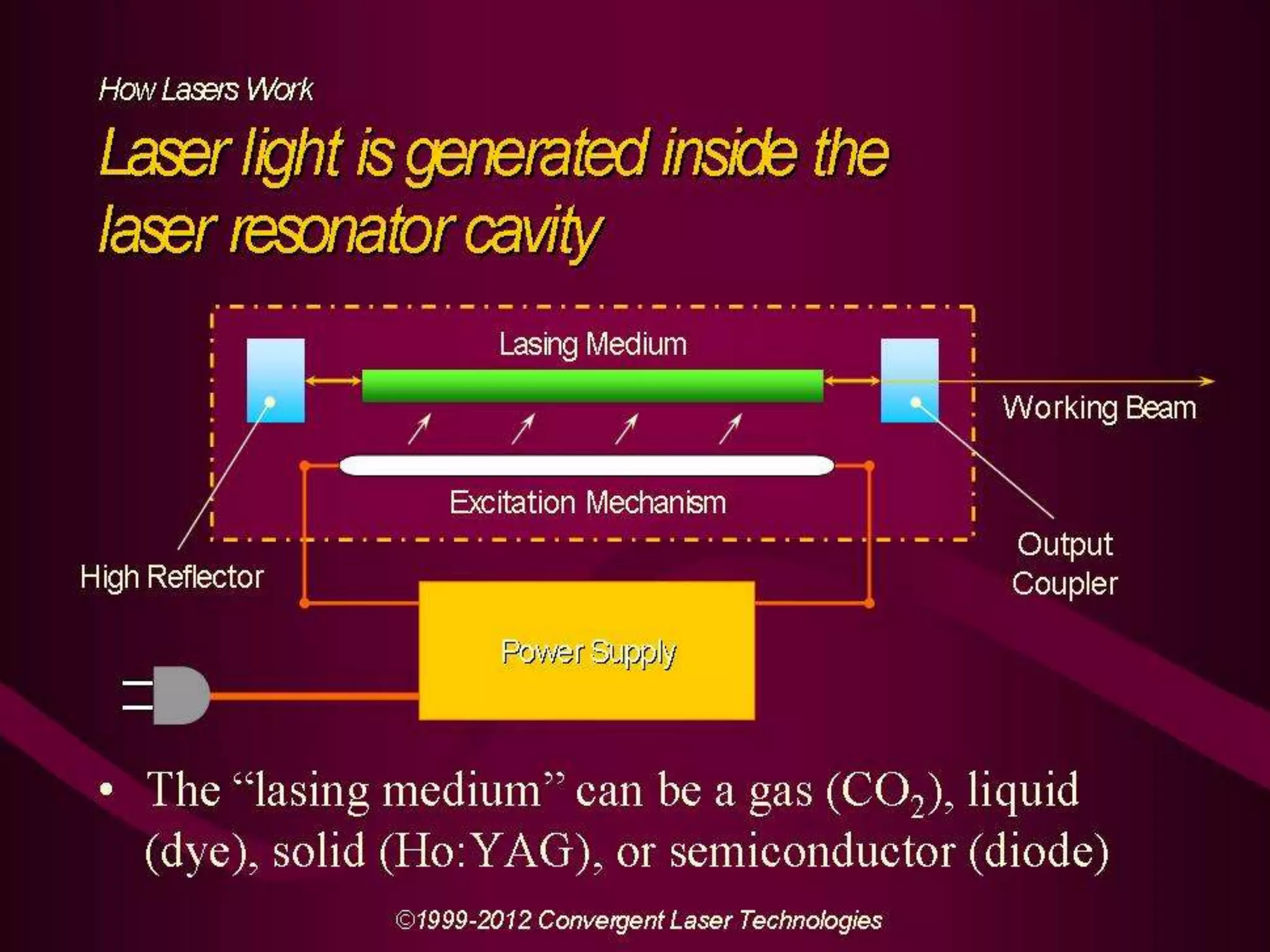
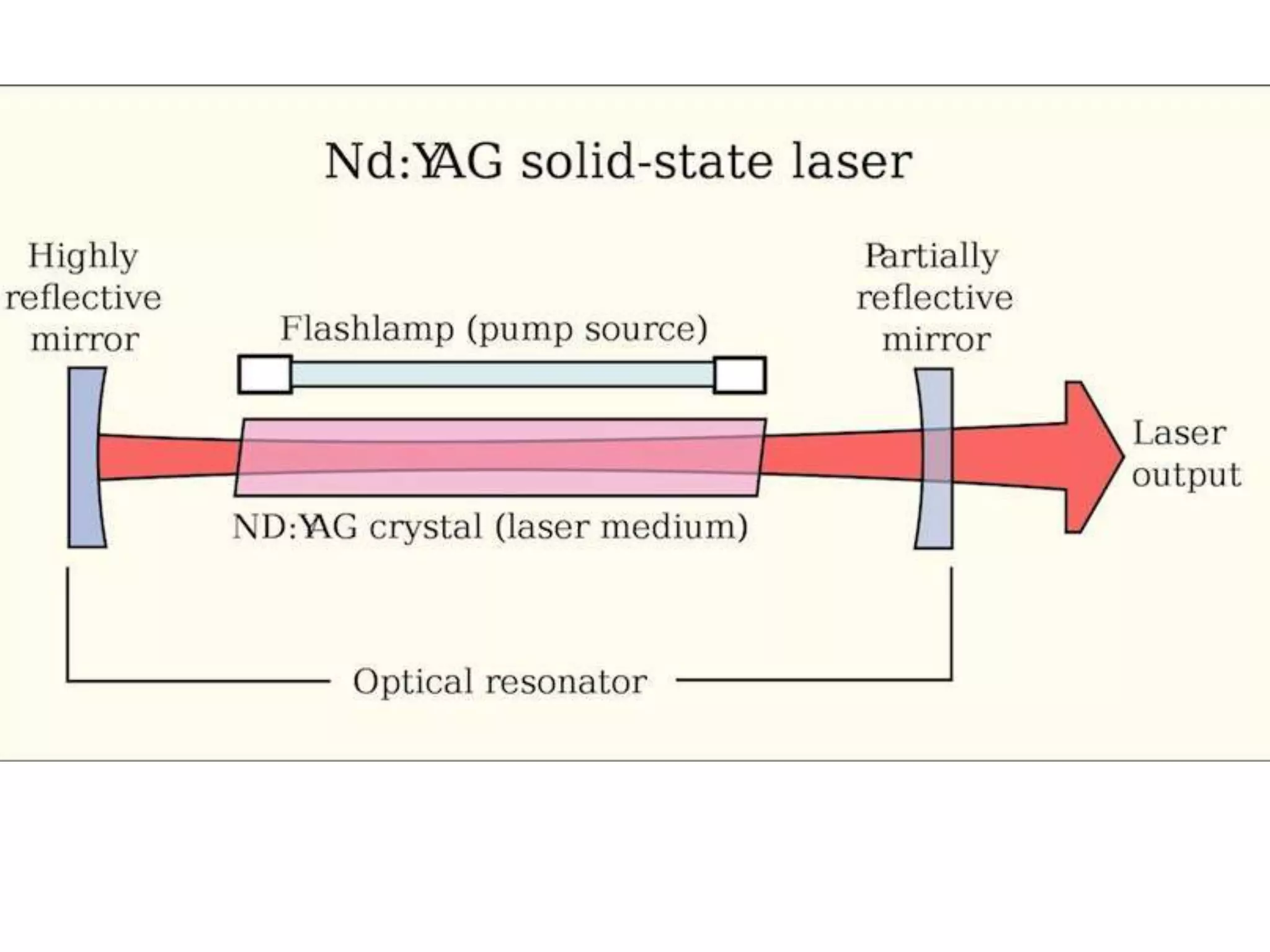
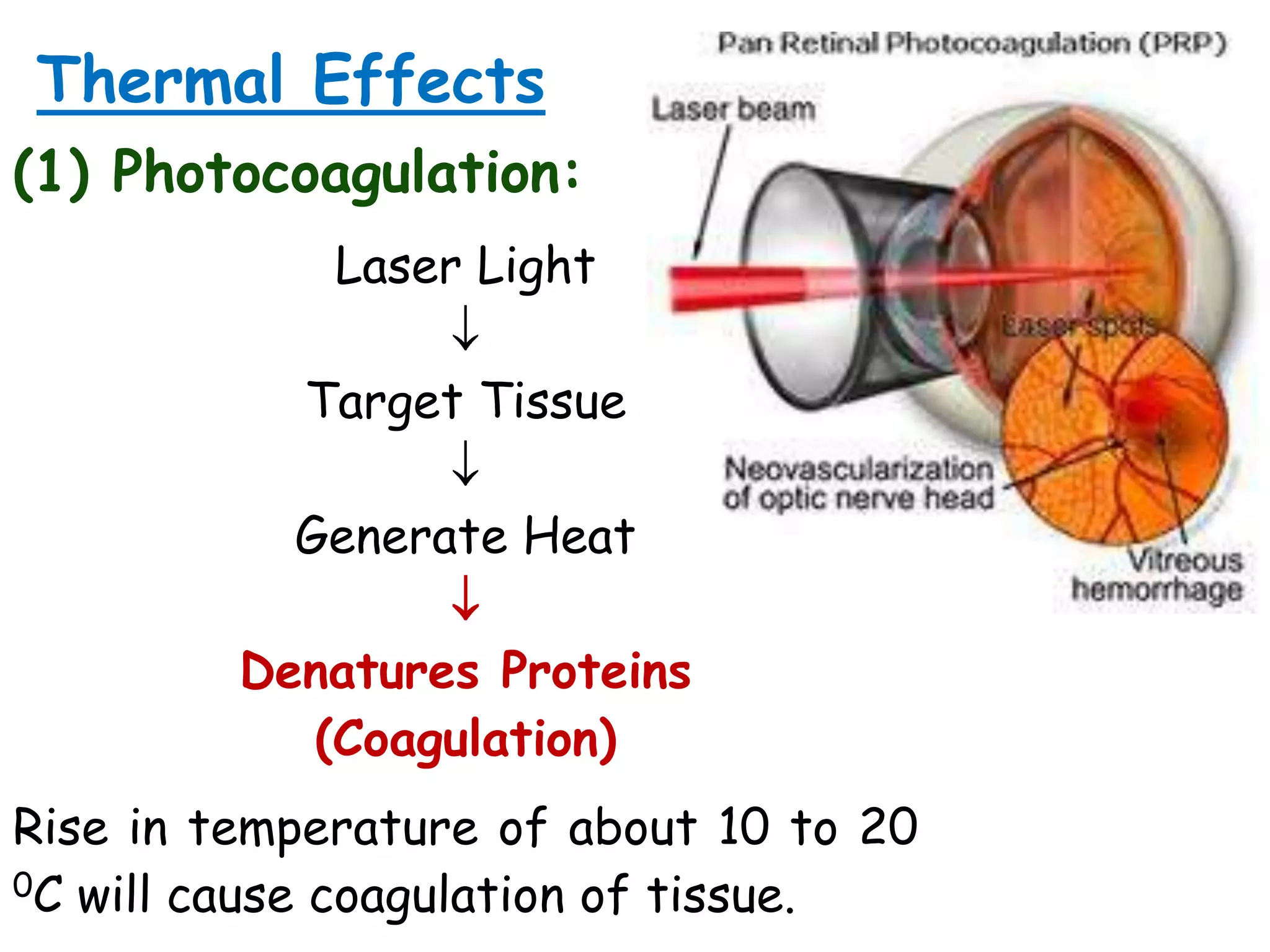
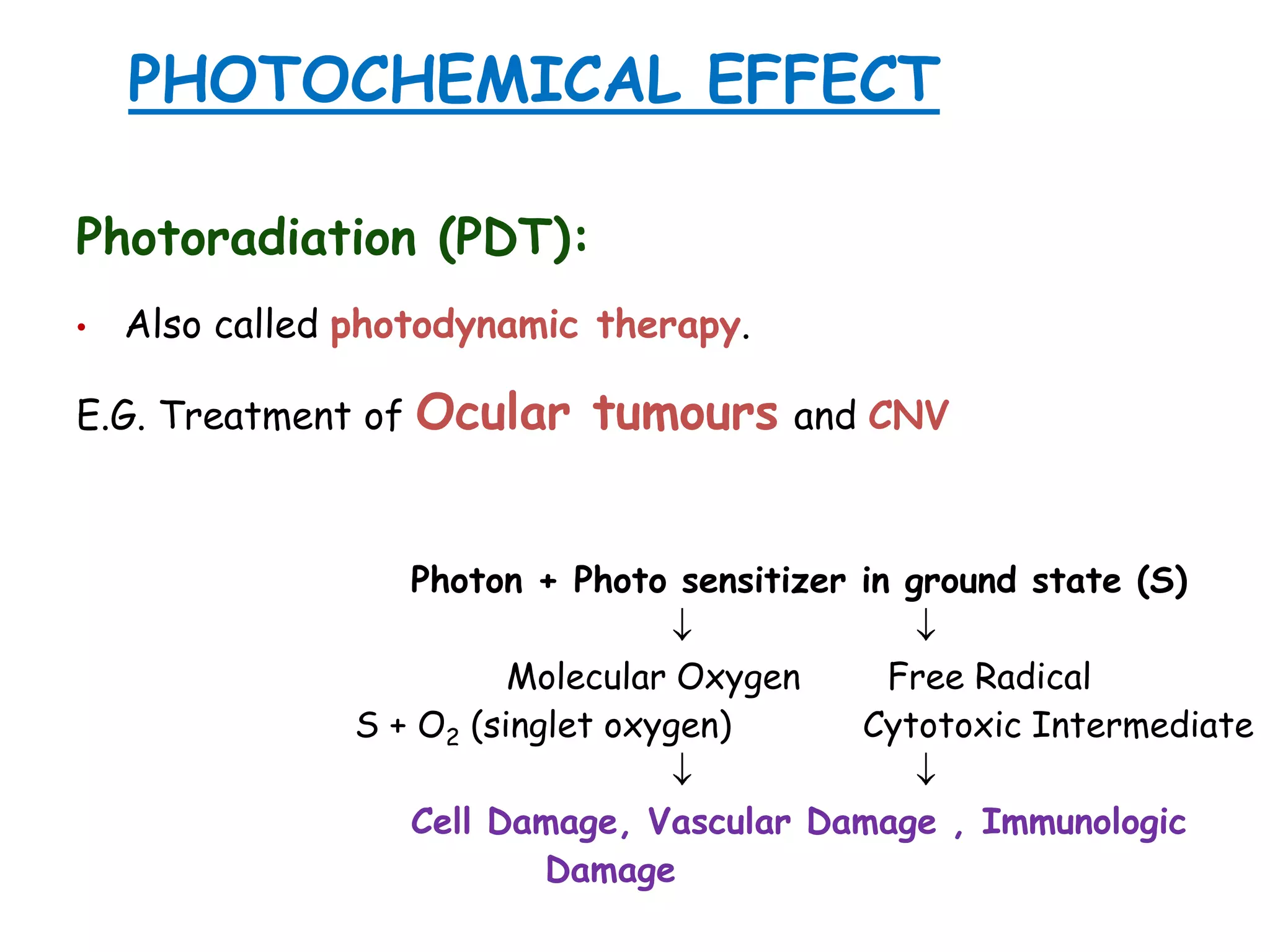
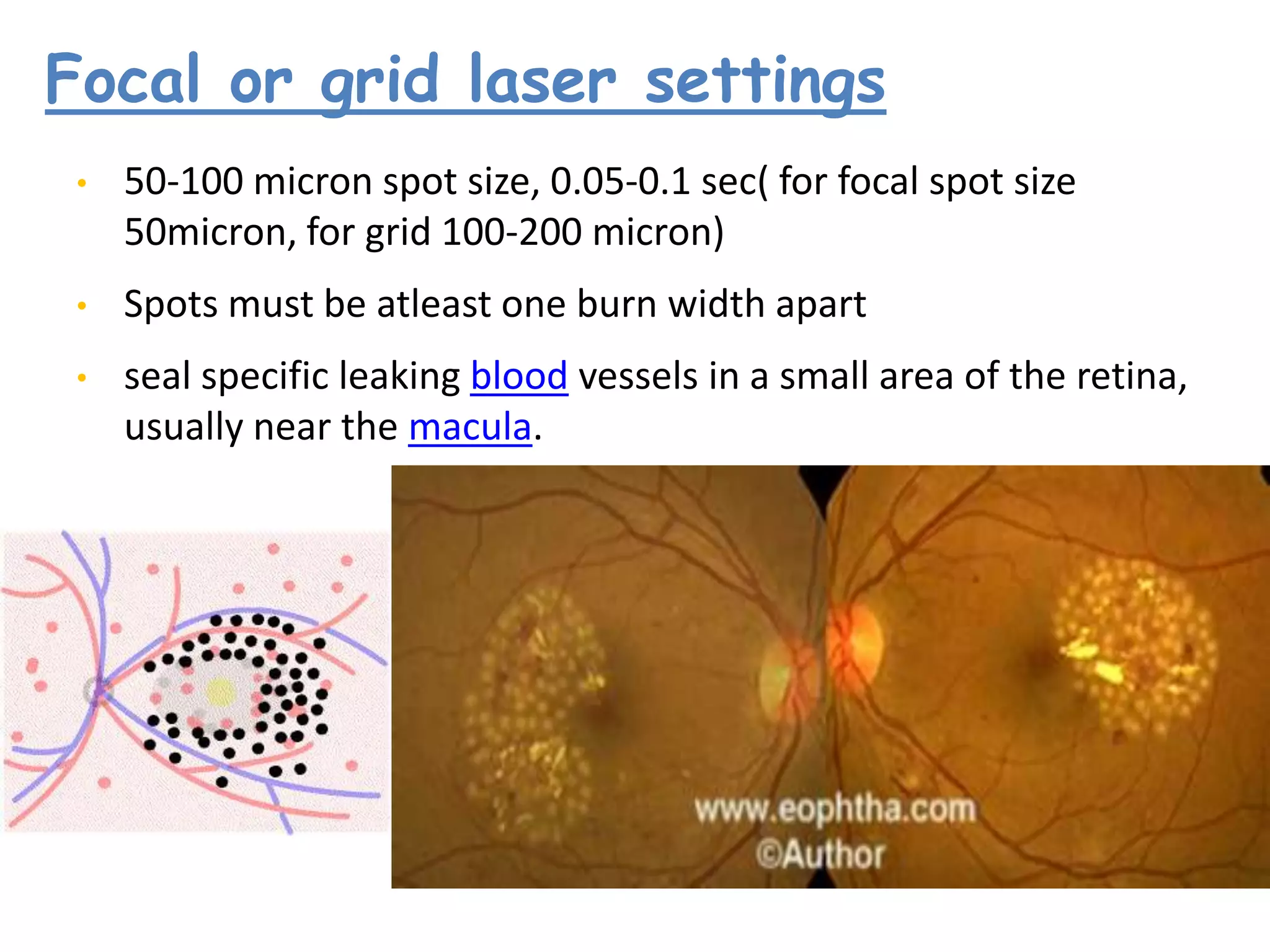
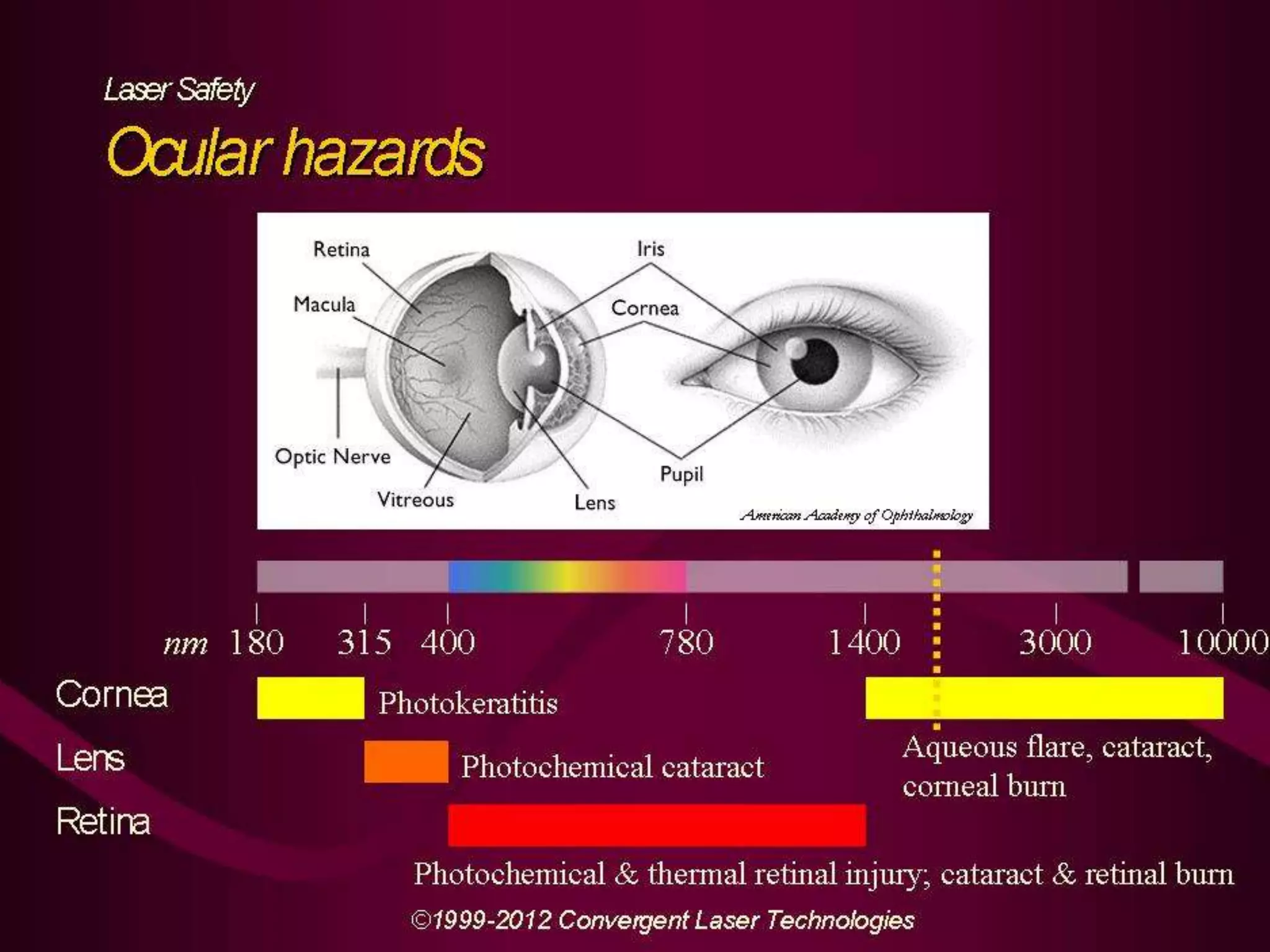
This document provides information about lasers and their use in ophthalmology. It begins with definitions of laser and its acronym. It then discusses the history and development of lasers from 1917 to present. The key properties and mechanisms of laser light production are described. Common types of ophthalmic lasers and their applications are outlined, including Nd:YAG, excimer, and diode lasers used for conditions like glaucoma, refractive error correction, and retinal diseases. The laser-tissue interaction mechanisms of thermal, photochemical and ionizing effects are summarized. The document concludes with sections on laser instrumentation and delivery systems and specific laser procedures in ophthalmology.