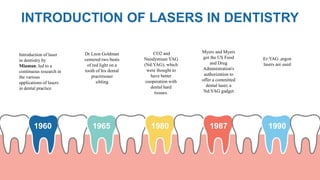
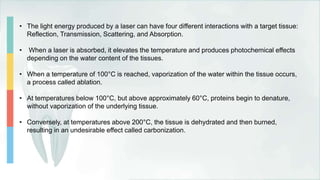
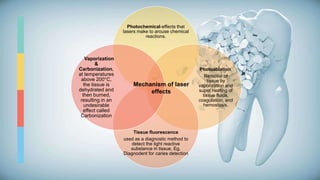
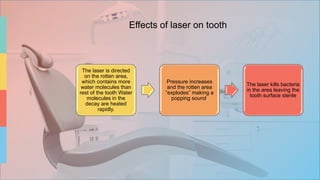
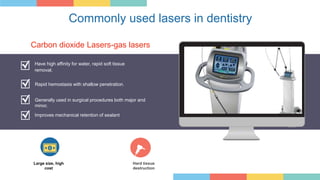
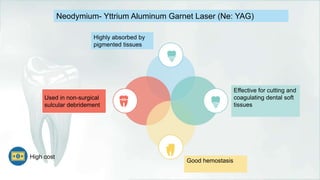
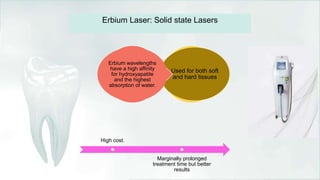
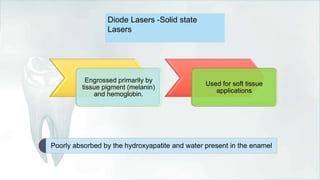
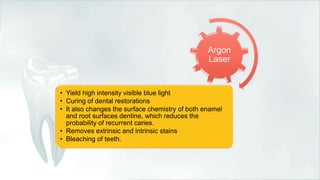
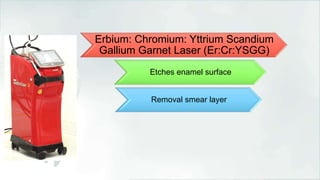
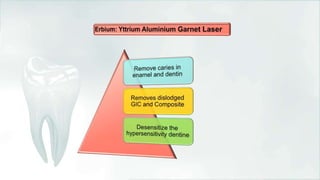
The document discusses the introduction and application of lasers in dentistry, including types such as CO2 and Nd:YAG lasers, and their mechanisms of action. It highlights their benefits, such as minimizing bleeding and promoting faster healing, as well as drawbacks, including limitations on certain dental materials and the need for anesthesia in some cases. The document concludes that while lasers cannot replace all conventional procedures, they offer innovative solutions that enhance patient care in dental practices.