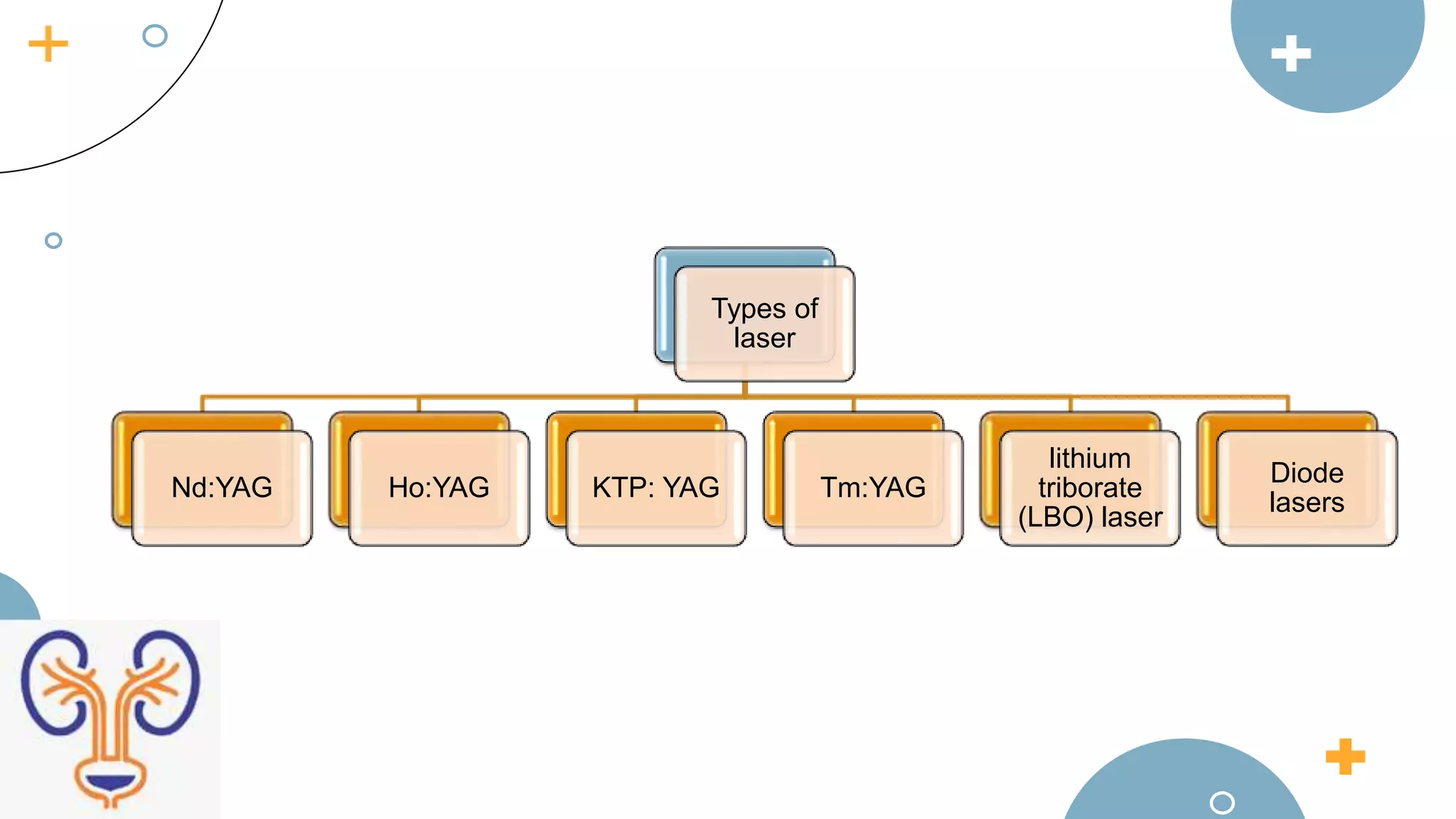
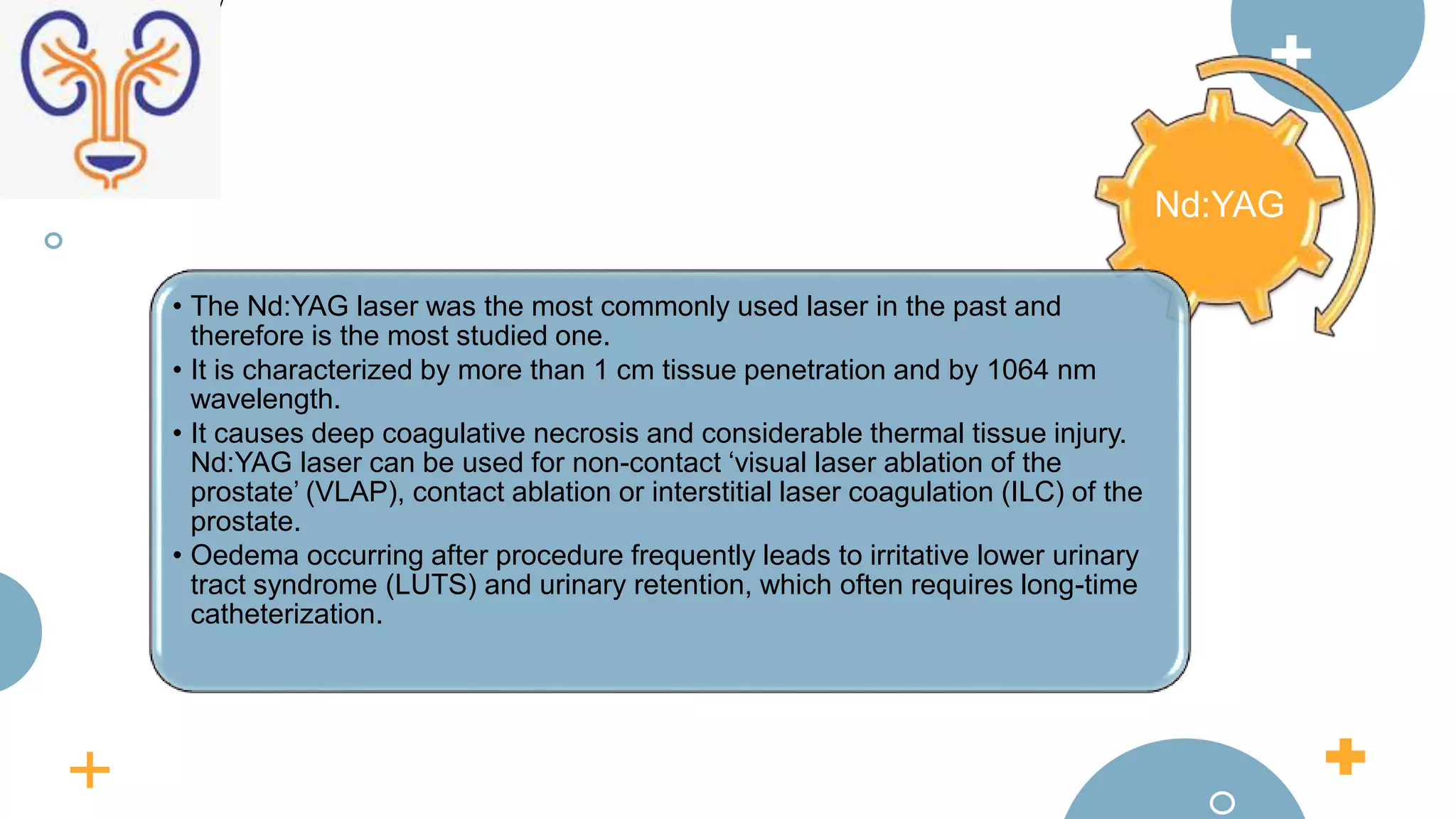
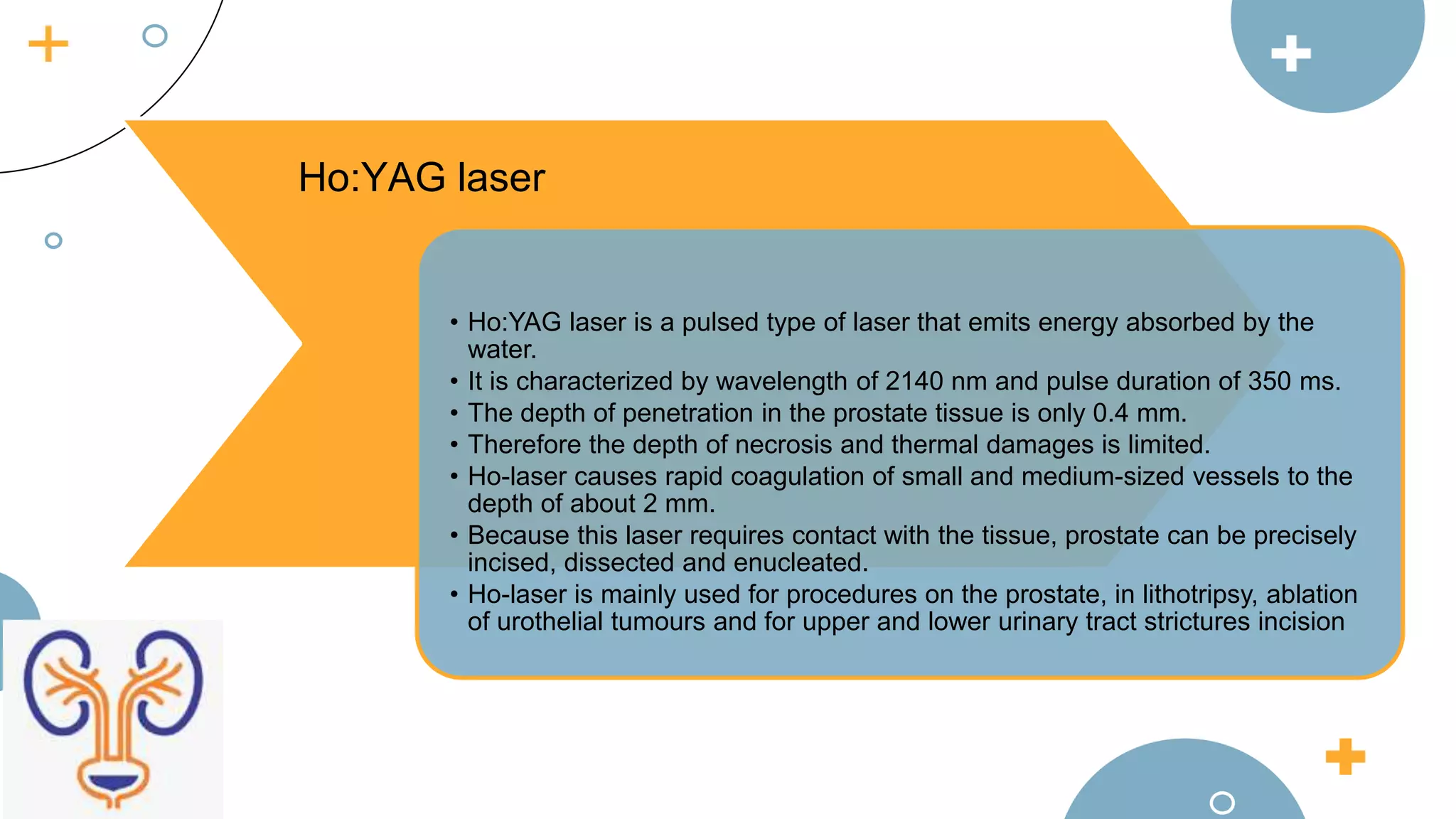
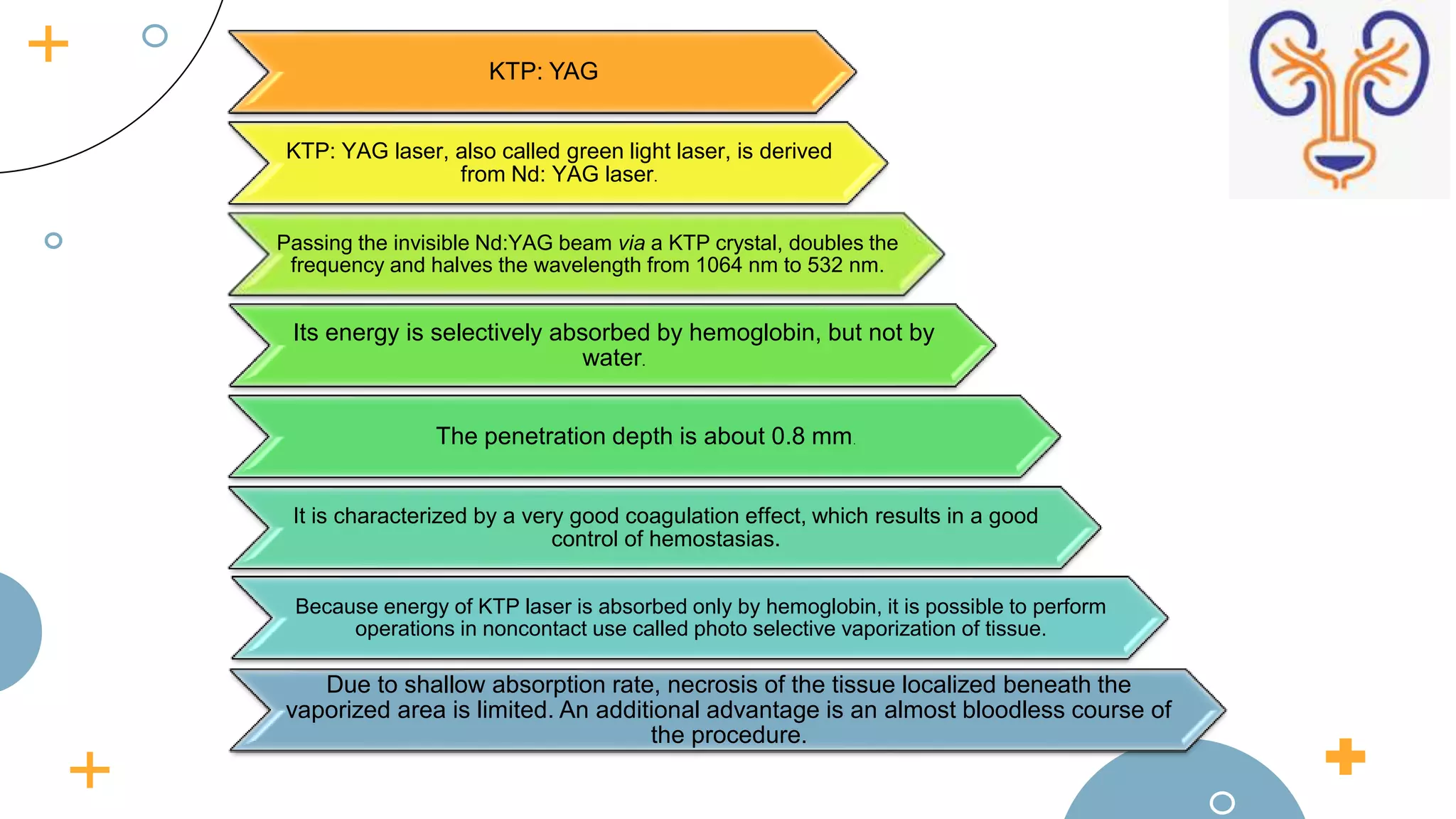
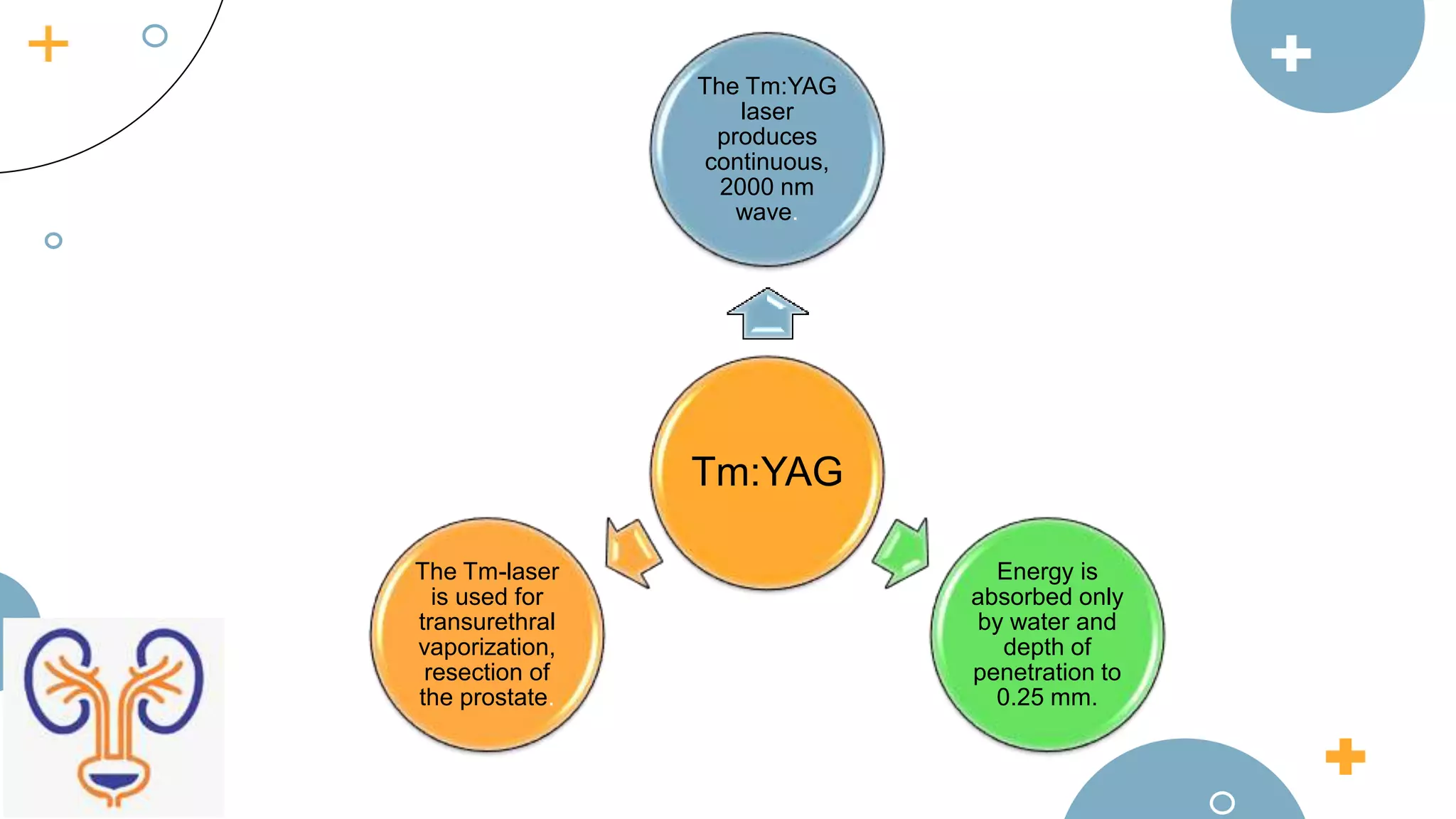
The document discusses the role of lasers in urology, highlighting their use in treating conditions such as benign prostatic hyperplasia and urinary tract cancers. It outlines the history and development of various laser technologies, their mechanisms, and specific applications in urologic procedures, including laser lithotripsy and prostate surgeries. Advancements in laser techniques have made them a popular alternative to traditional surgical methods due to improved efficacy and reduced complications.