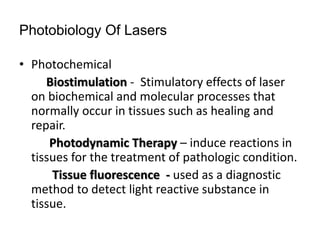
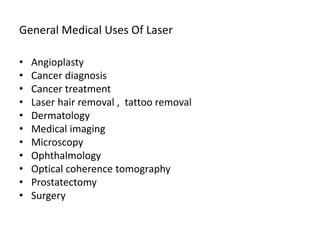
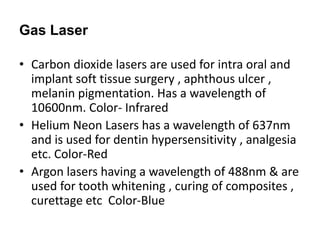
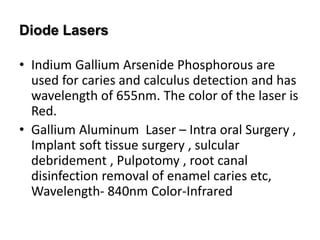
This document discusses the use of lasers in dentistry. It begins with an introduction and history of lasers, then covers the fundamentals of laser operation and classification of lasers. The main uses of lasers in dentistry include soft tissue procedures like biopsy and surgery. Techniques for ablation, vaporization, and low level laser therapy are described. Benefits are reduced pain and bleeding, while risks include hazards to patients and staff if not used properly. Proper safety protocols and sterilization of laser equipment are emphasized.

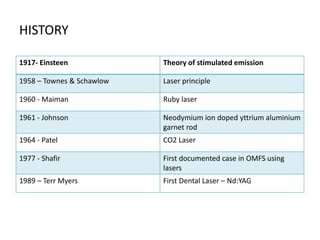
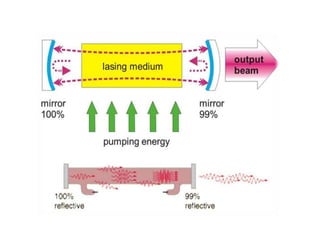
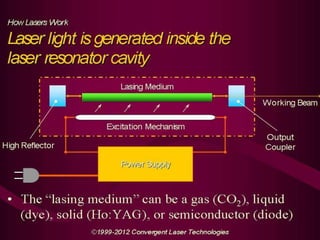
![Fundamentals Of Laser Operation
• Components -
Active medium [ Lasing Medium ]
Pumping mechanism
Optical Resonators
Laser Delivery System
Cooling system
Control Panel](https://image.slidesharecdn.com/presentation1-140617104943-phpapp01/85/Lasers-and-Its-Use-In-Dentistry-6-320.jpg)
![• Lasers are also used in arthroscopic
surgery of TMJ
• Scar revision is also made possible
these days with the help of pulsed dye
lasers[PDL]. PDL have hb as their
chromophores and penetrate the
epidermis without de-epithelisation.
They reduce scar tissue erythema and
induce collagen remodeling to flatten
and soften scars. Indicated in cases](https://image.slidesharecdn.com/presentation1-140617104943-phpapp01/85/Lasers-and-Its-Use-In-Dentistry-33-320.jpg)