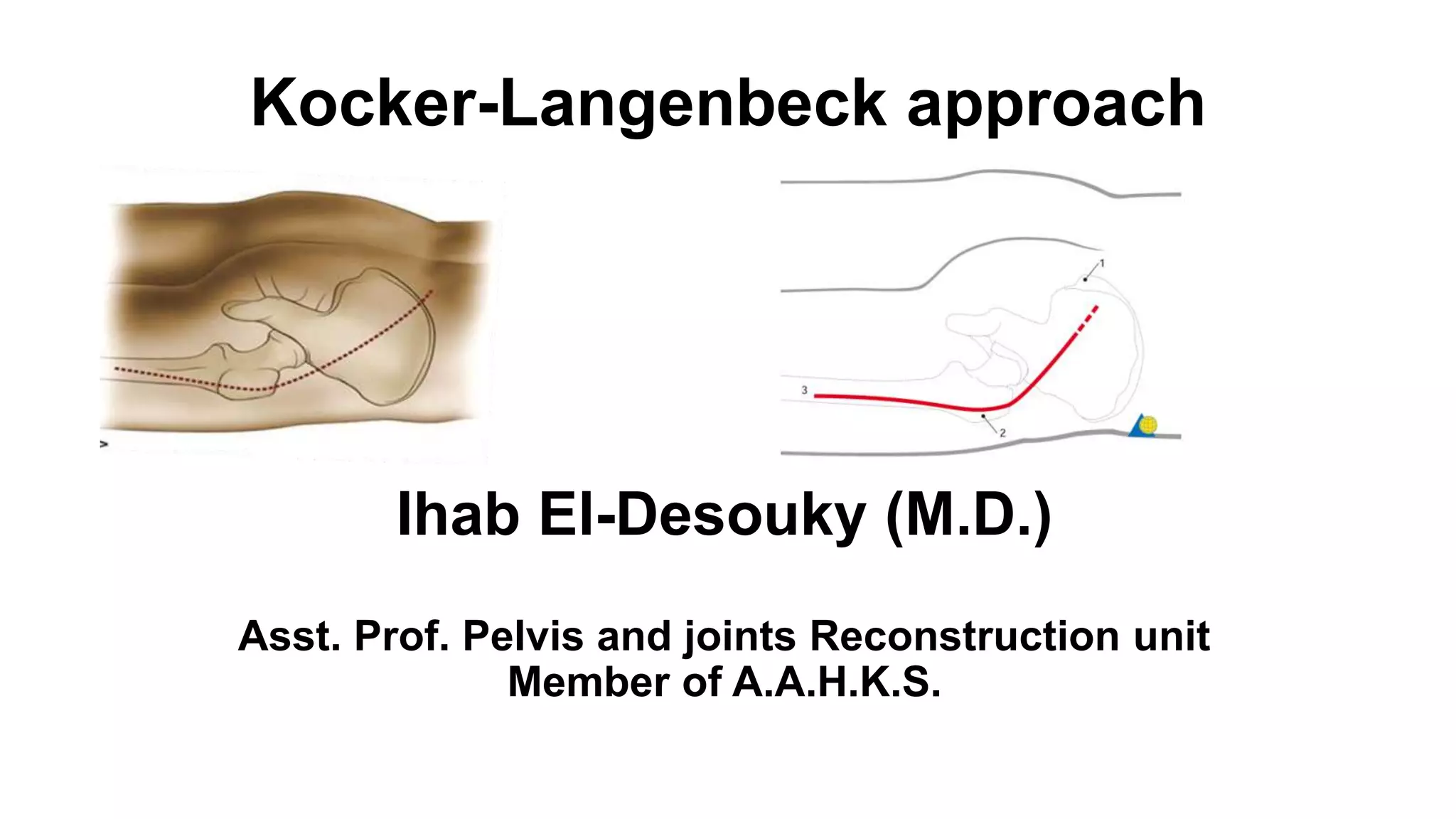
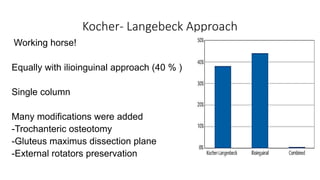
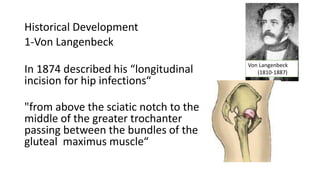
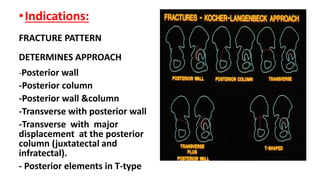
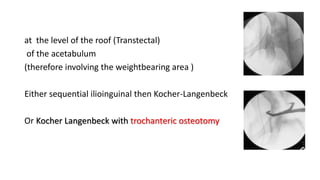
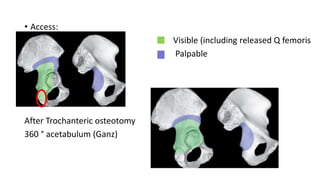
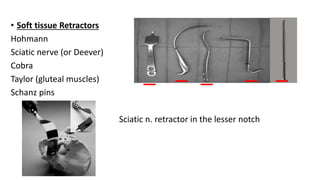
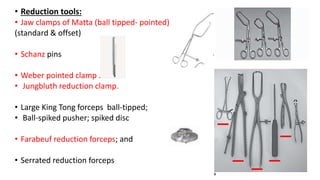
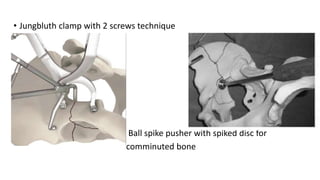
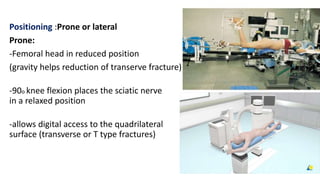
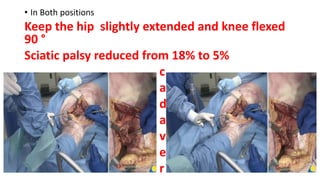
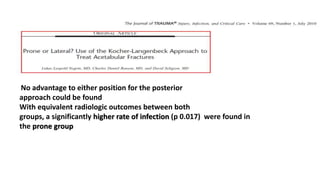
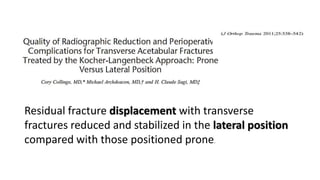
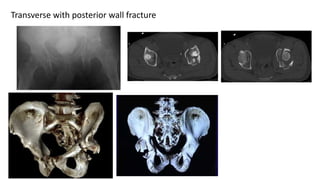
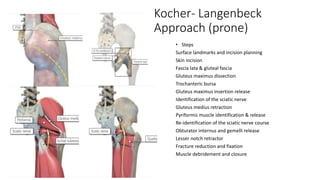
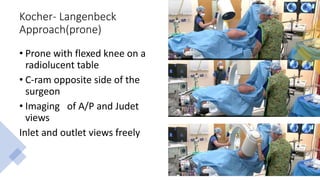
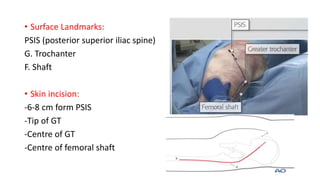
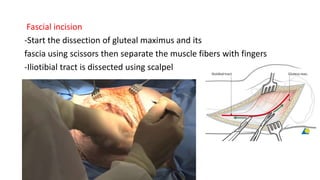
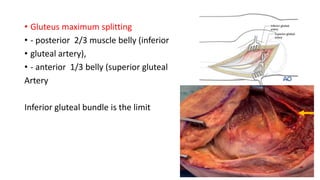
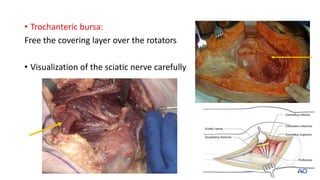
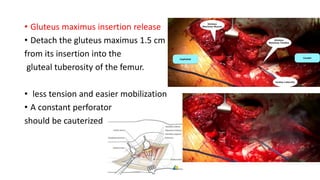
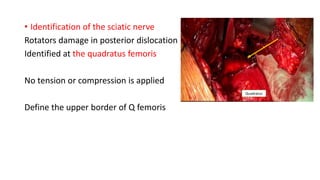
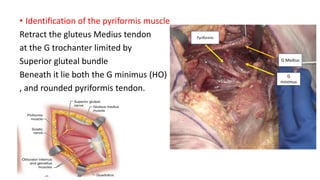
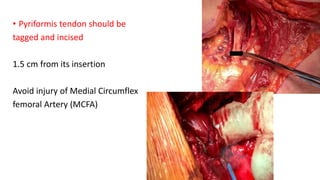
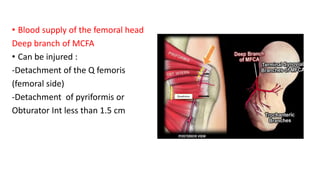
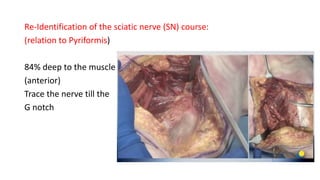
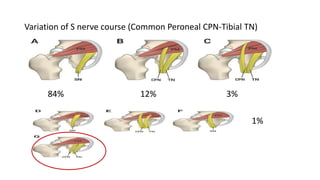
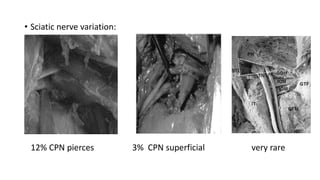
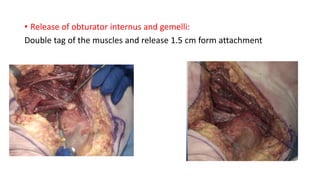
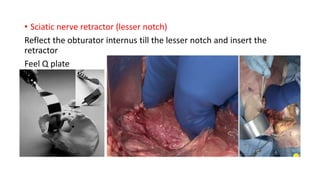
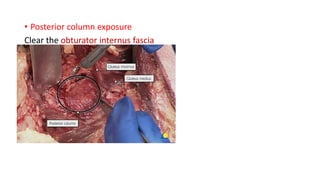
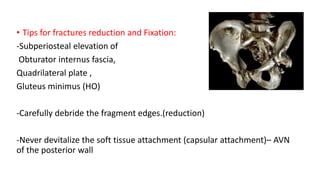
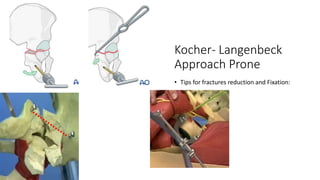
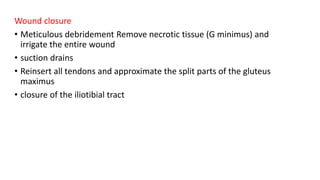
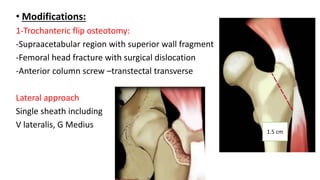
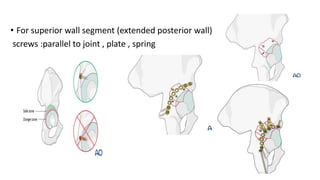
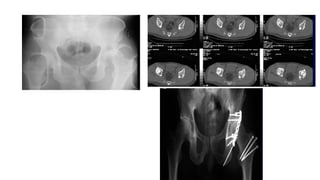
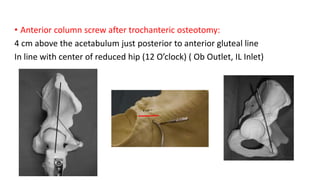
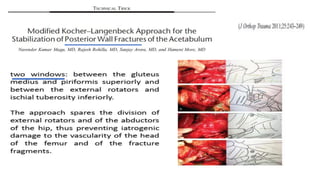
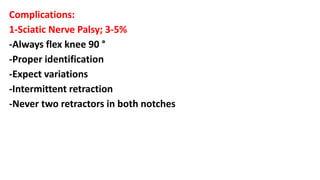
The document discusses the Kocker-Langenbeck surgical approach for hip fractures. It provides a brief history of the approach's development. The key steps of the classic approach are described, including indications, positioning, incision, exposure of anatomical structures, fracture reduction techniques, and potential complications. Modifications like trochanteric osteotomy are also covered. The approach remains a workhorse for treating posterior hip fractures but requires careful exposure and identification of structures to minimize risks.