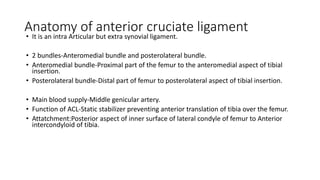
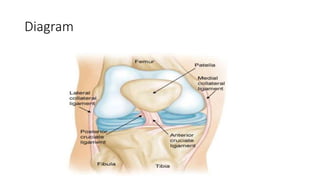
An ACL tear was described, including anatomy, biomechanics, causes, diagnosis, and treatment. Key points:
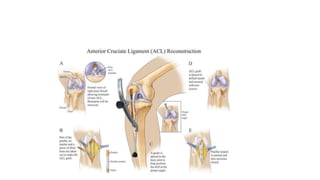
- The ACL has two bundles that stabilize the knee by preventing anterior tibial translation. It is commonly injured in sports involving sudden stops or changes in direction.
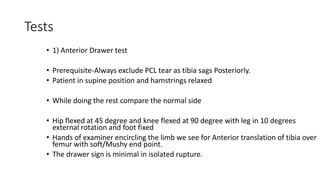
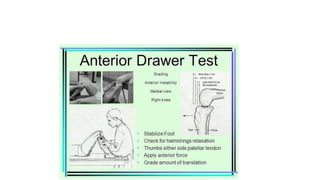
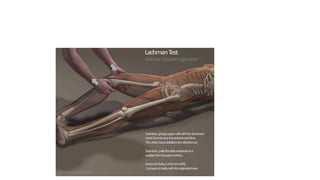
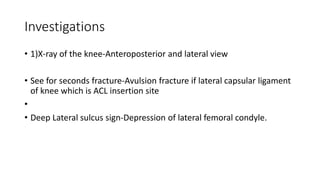
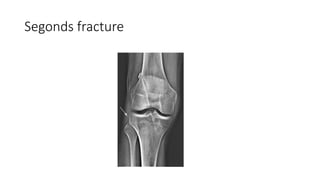
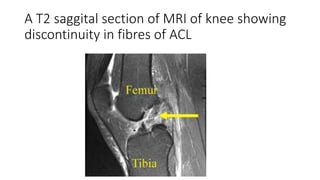
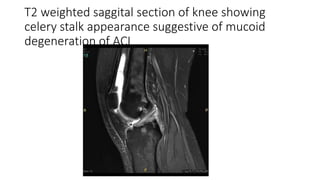
- Diagnosis involves clinical exams like the Lachman and pivot shift tests and MRI to confirm complete tear. ACL tears are often associated with meniscal injuries.
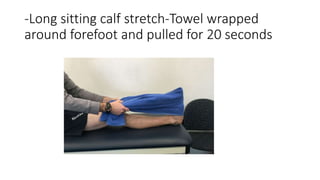
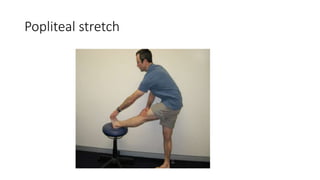
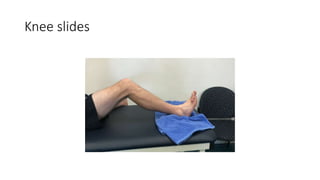
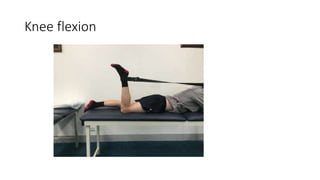
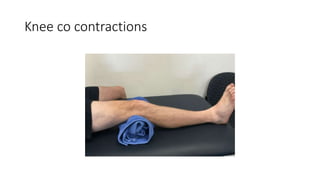
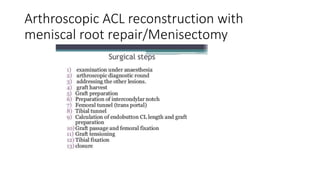
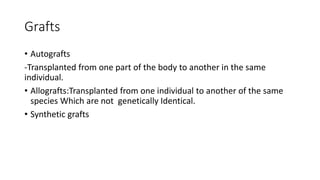
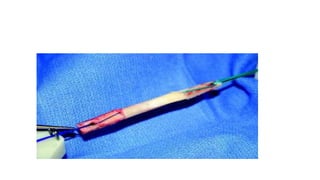
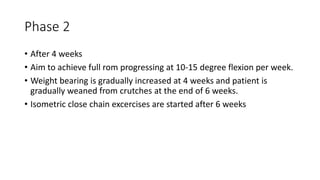
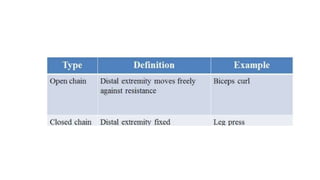
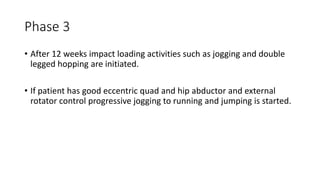
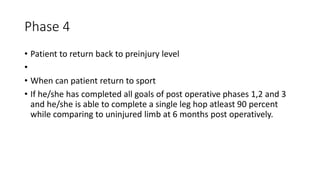
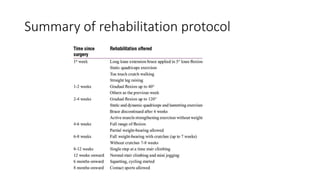
- Treatment includes initial RICE and bracing followed by physical therapy. Surgery with autograft reconstruction using the patellar tendon or hamstrings is recommended for active individuals to restore stability. Post-op rehabilitation progresses through phases of range of motion and strength training over 6-12 months