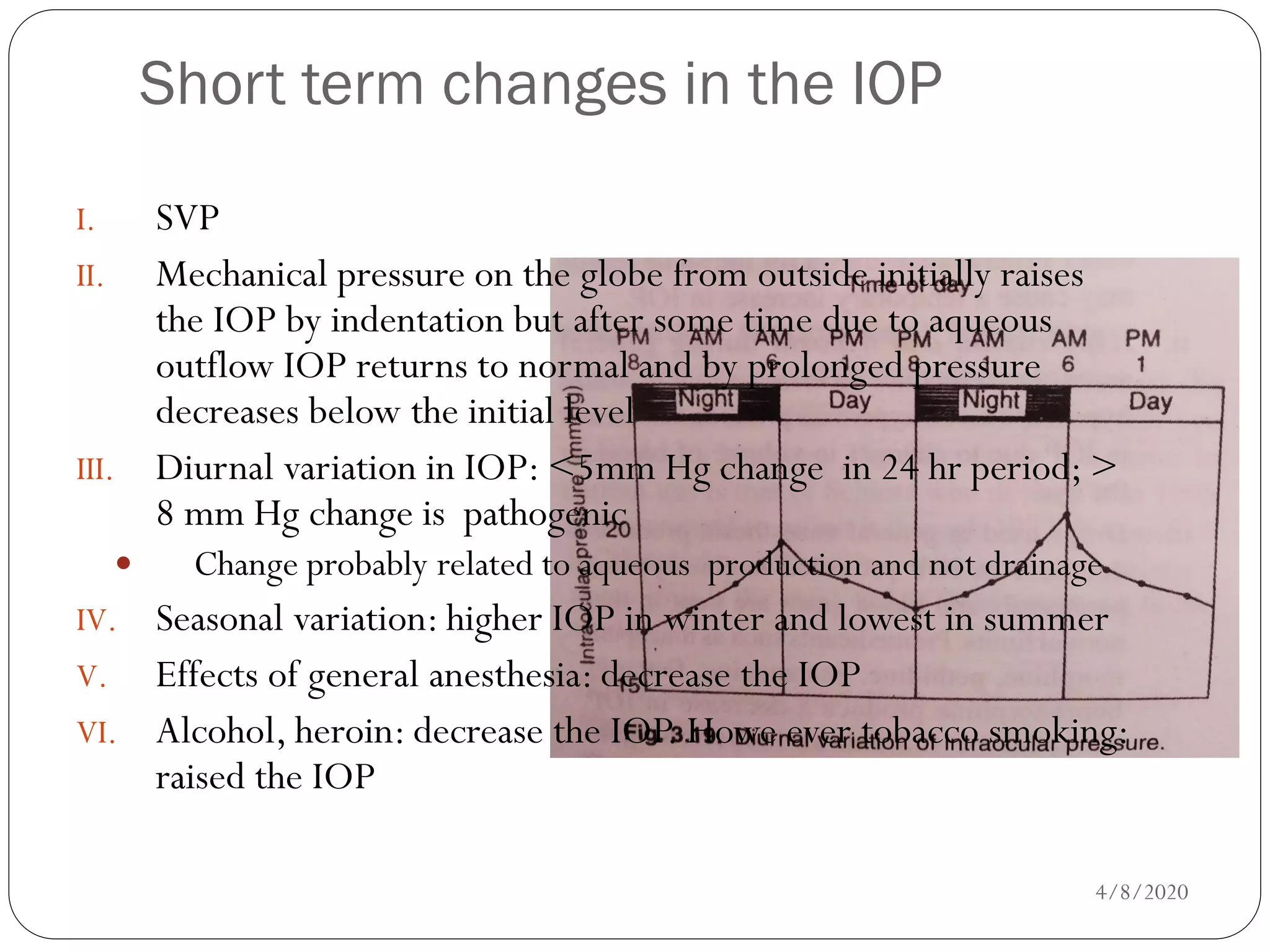
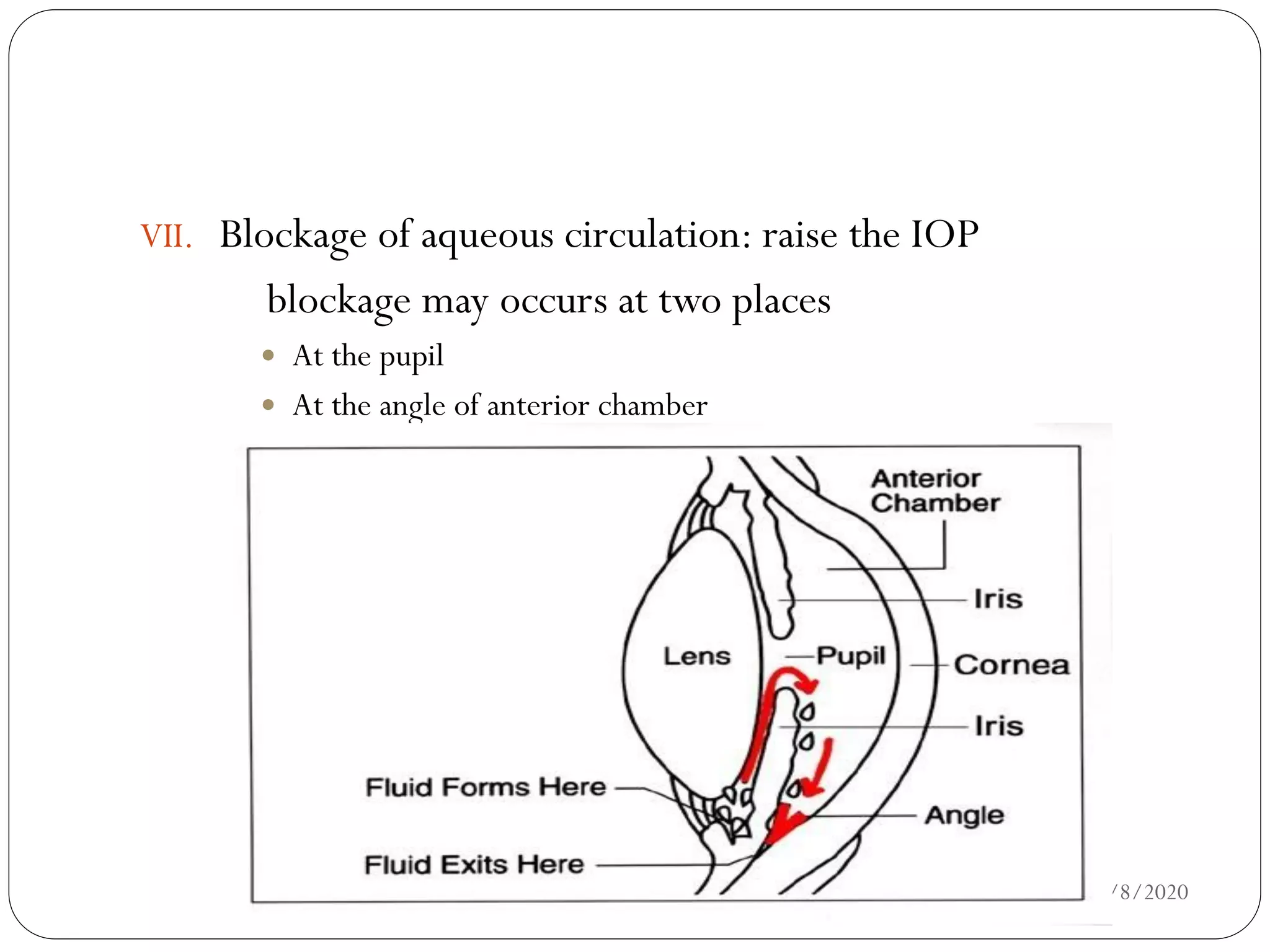
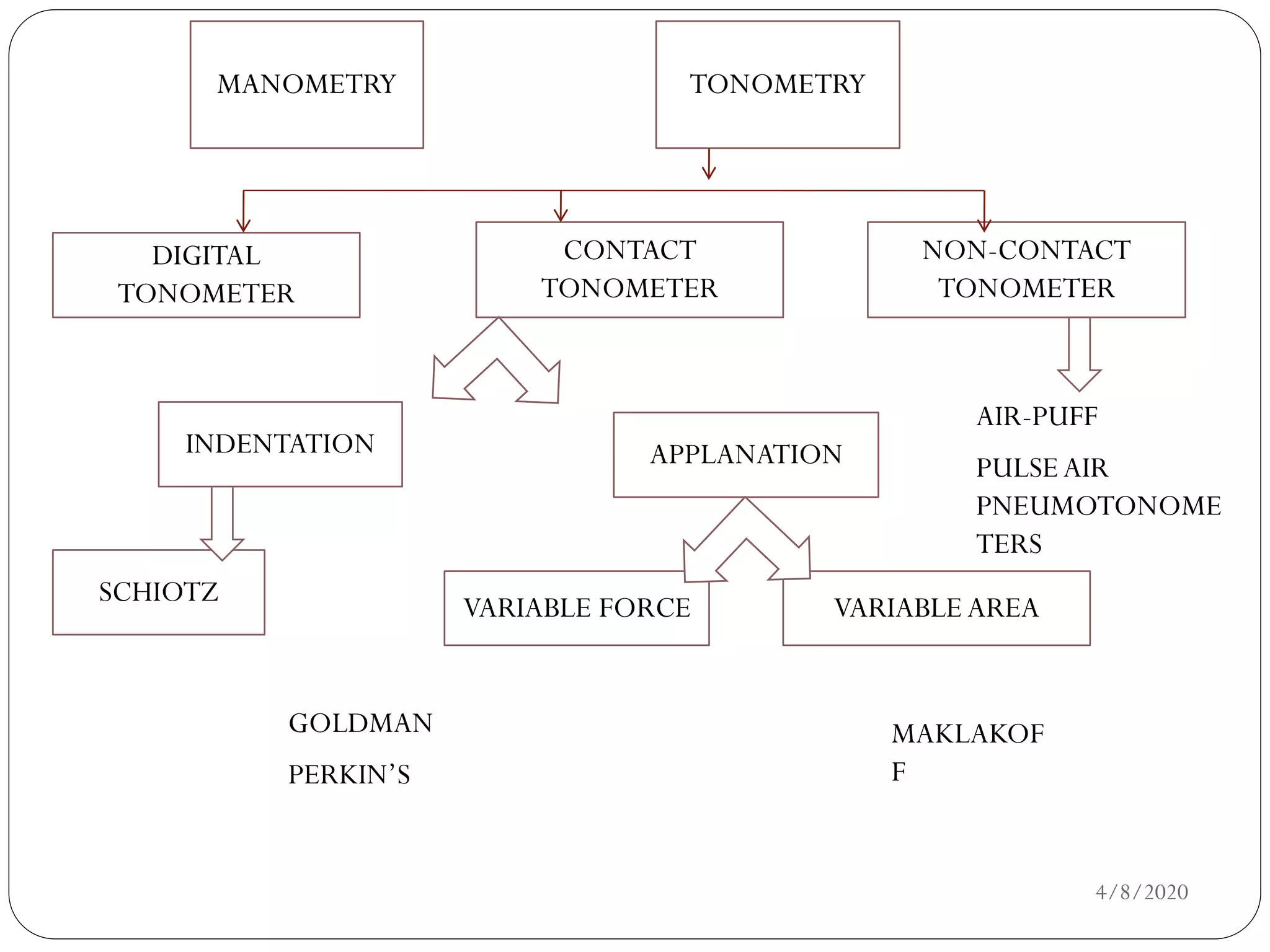
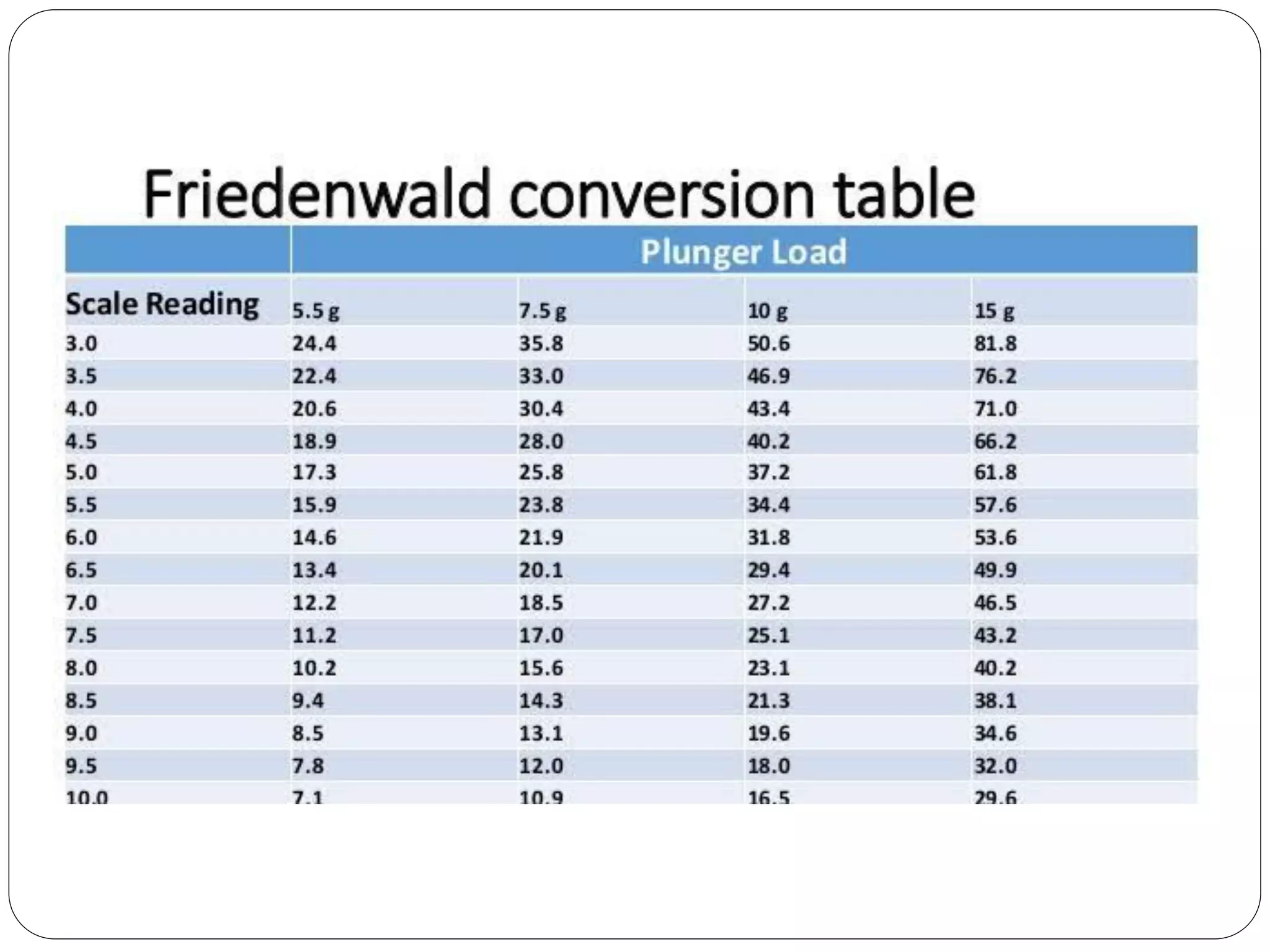
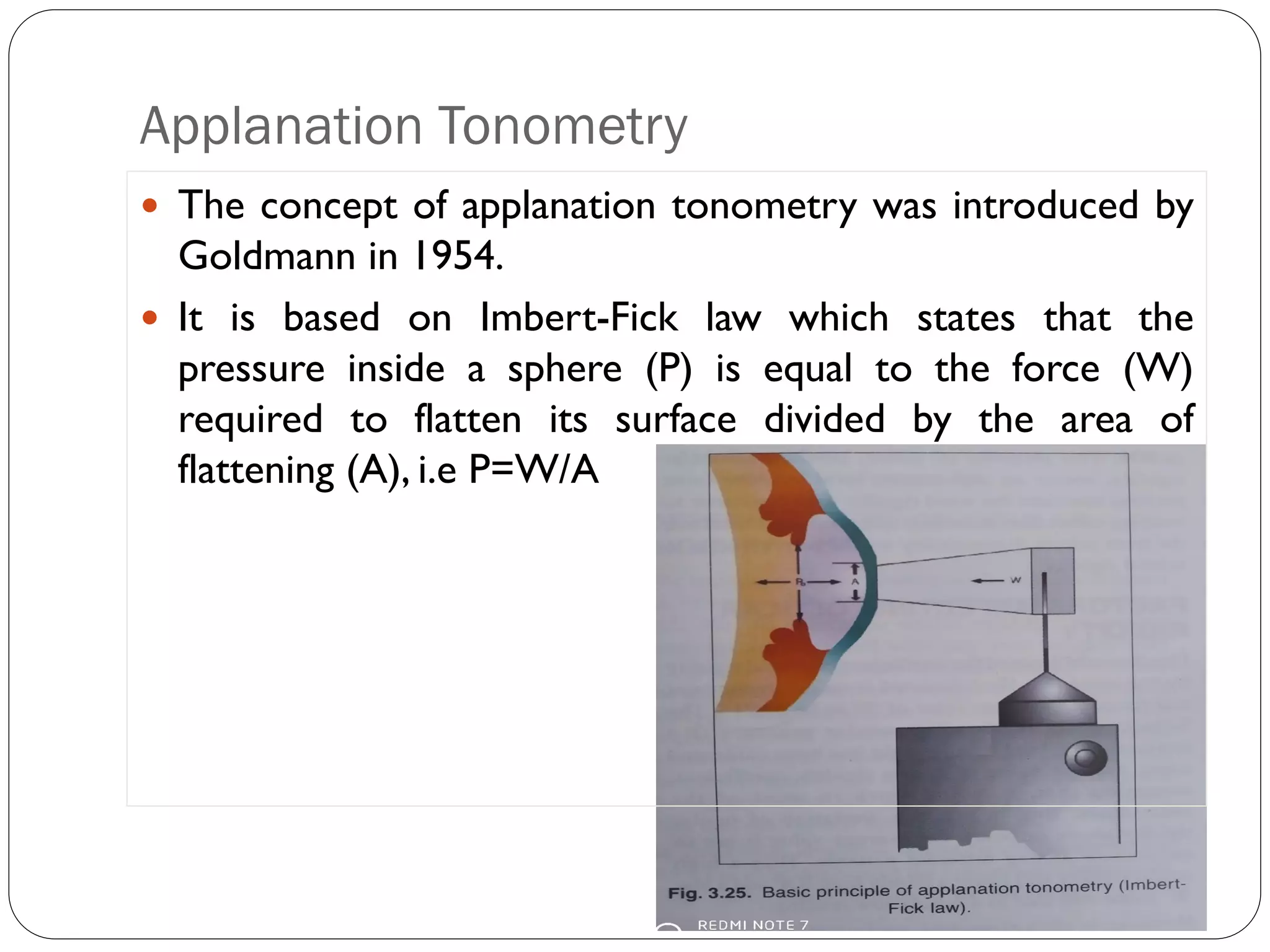
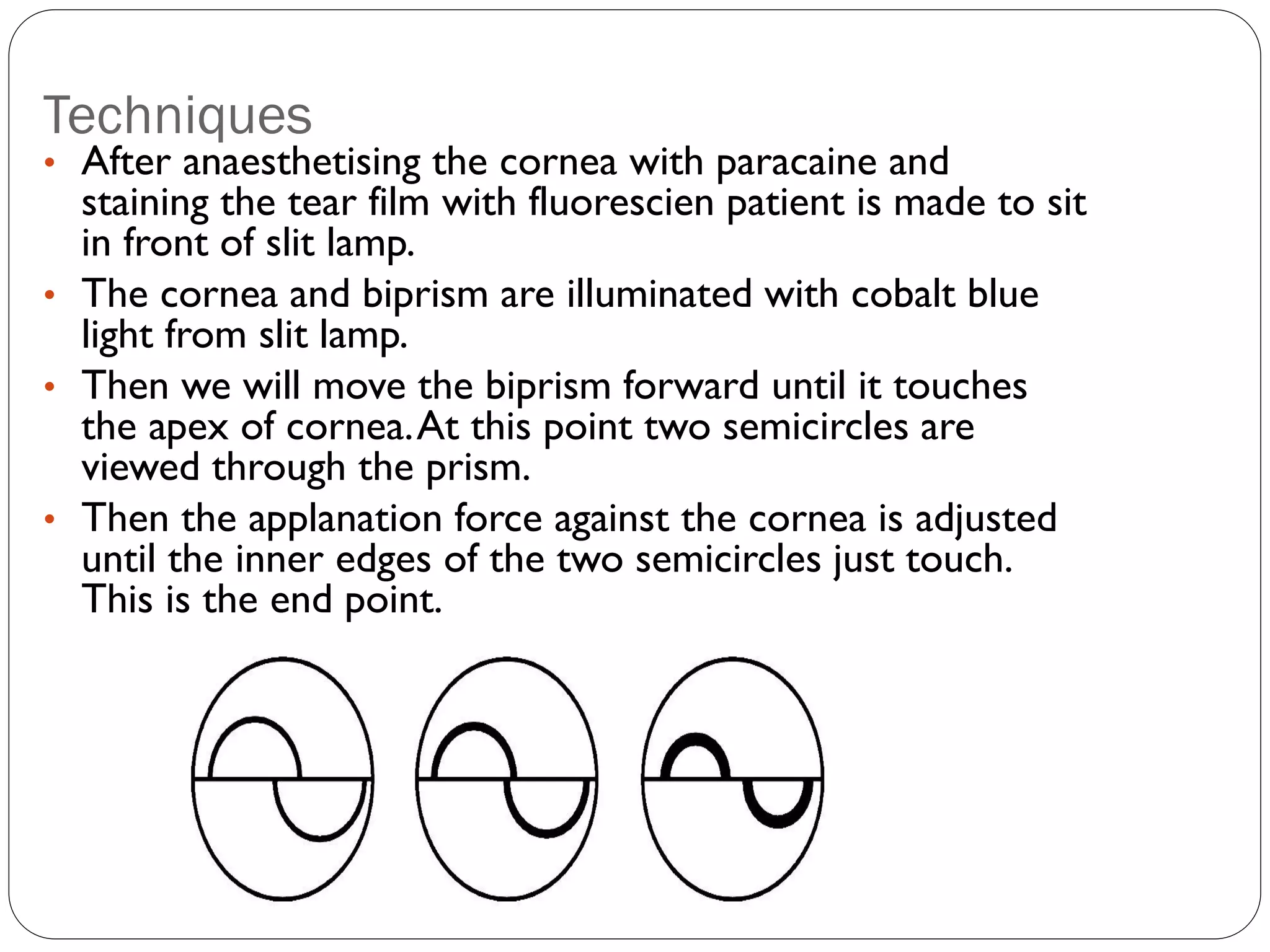
The document discusses intraocular pressure (IOP) and methods of measuring IOP (tonometry). It defines IOP as the fluid pressure inside the eye and notes the normal range is 10.5-20.5 mmHg. Factors that can influence IOP include heredity, age, drugs, and blockage of aqueous circulation. Common tonometry methods are discussed - indentation tonometry uses a plunger like the Schiotz tonometer, while applanation tonometry is based on flattening the cornea and includes Goldmann, Perkins, and air puff tonometers. Accurate IOP measurement is important for evaluating glaucoma patients.