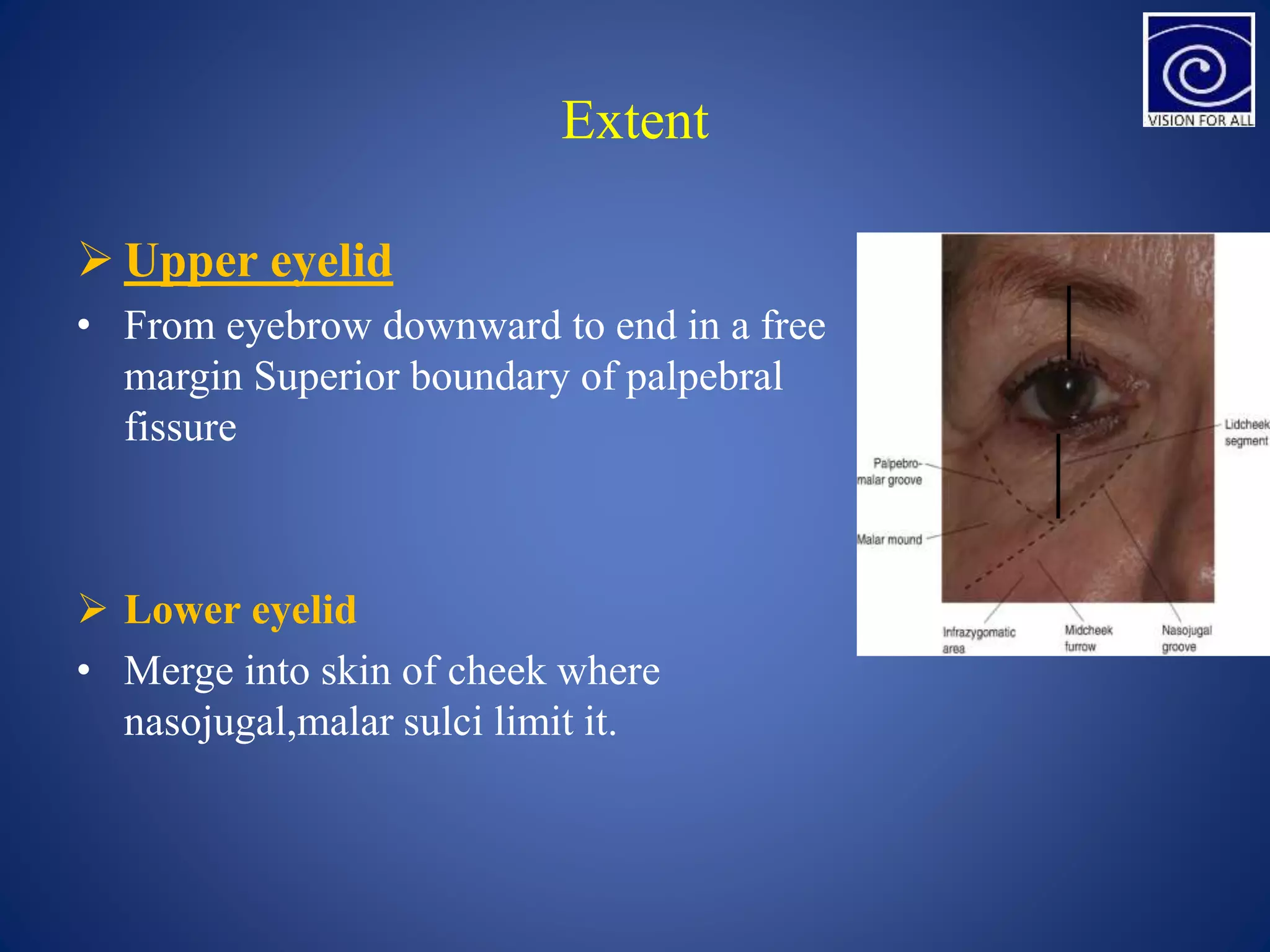
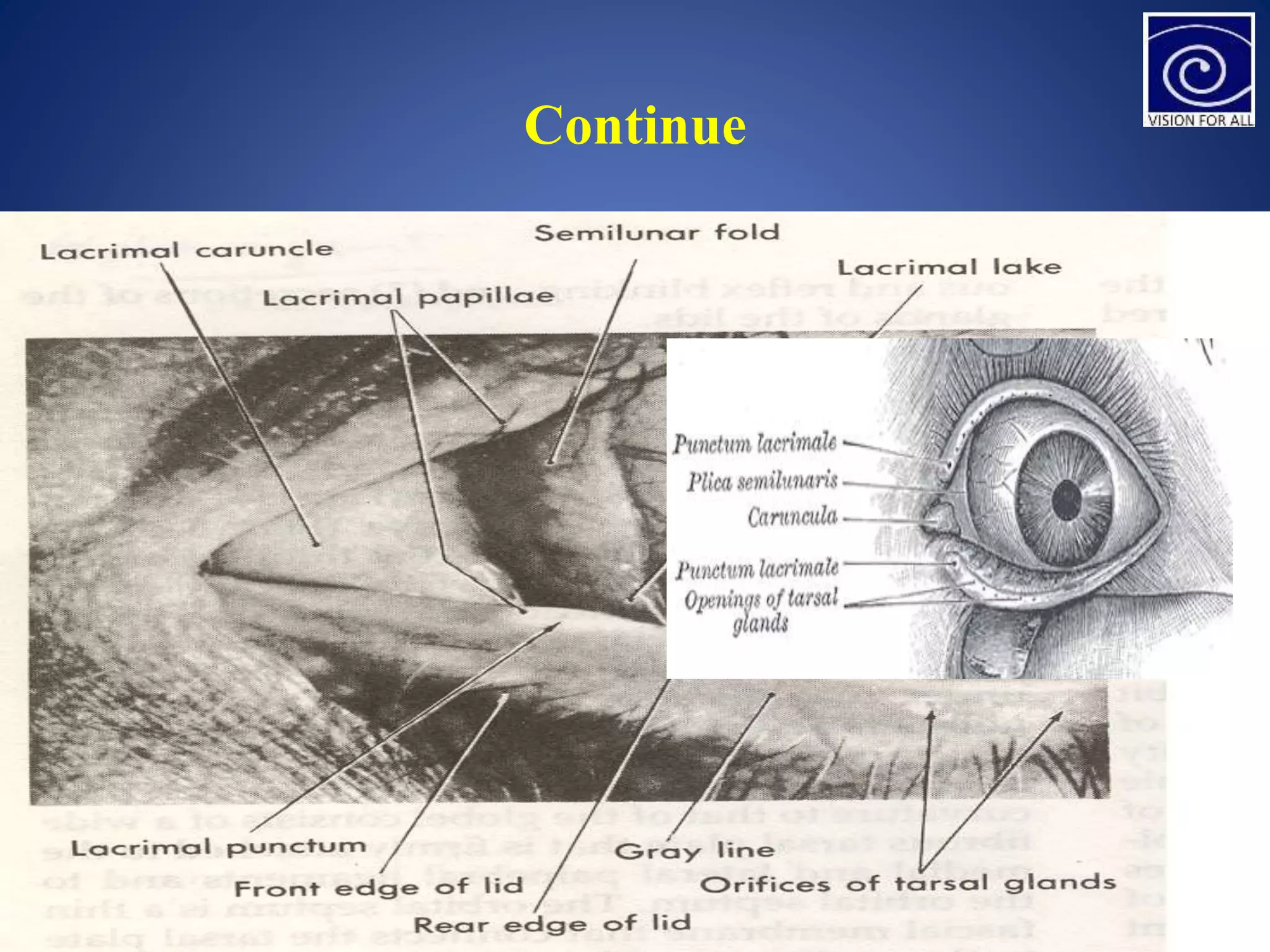
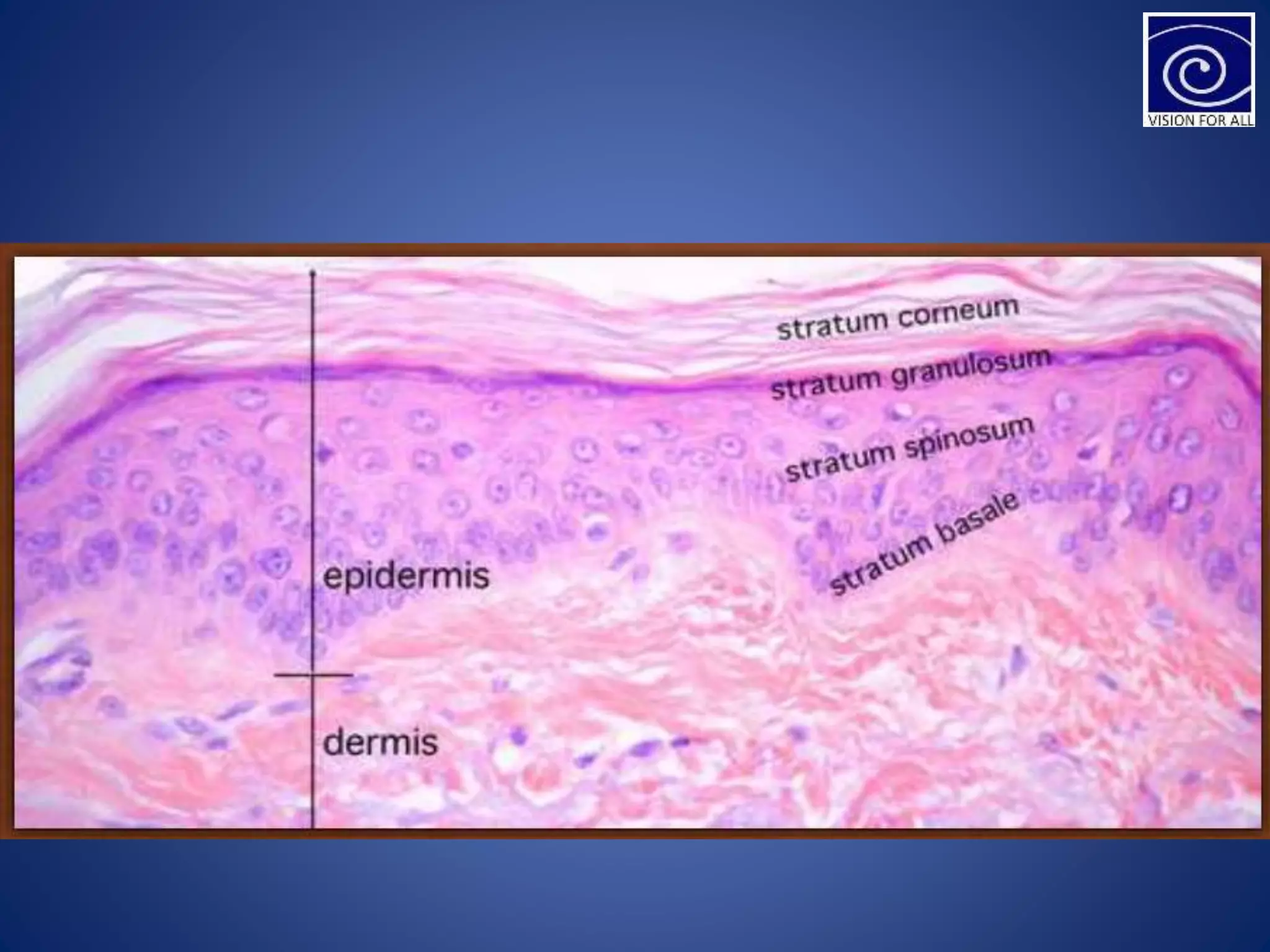
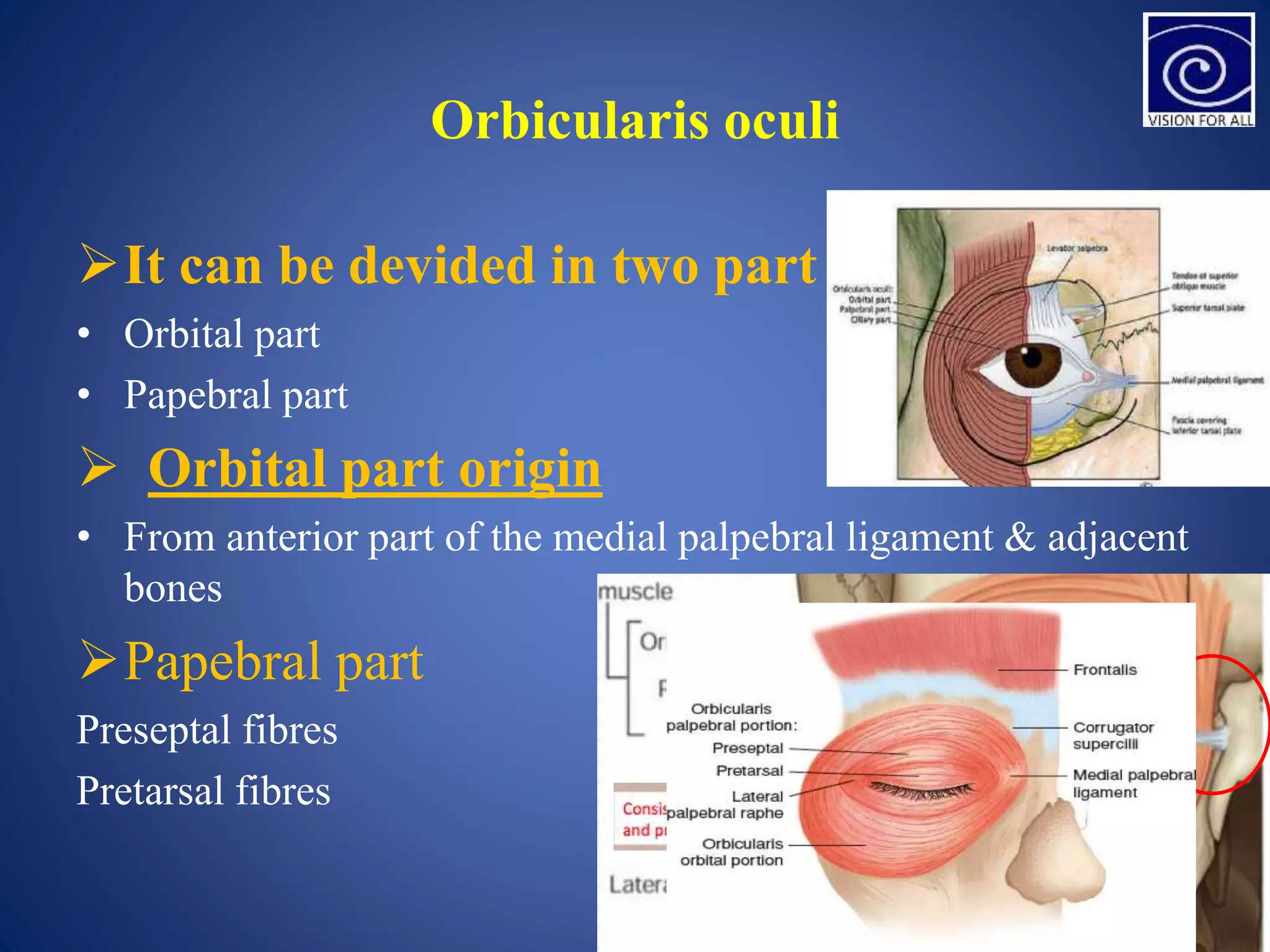
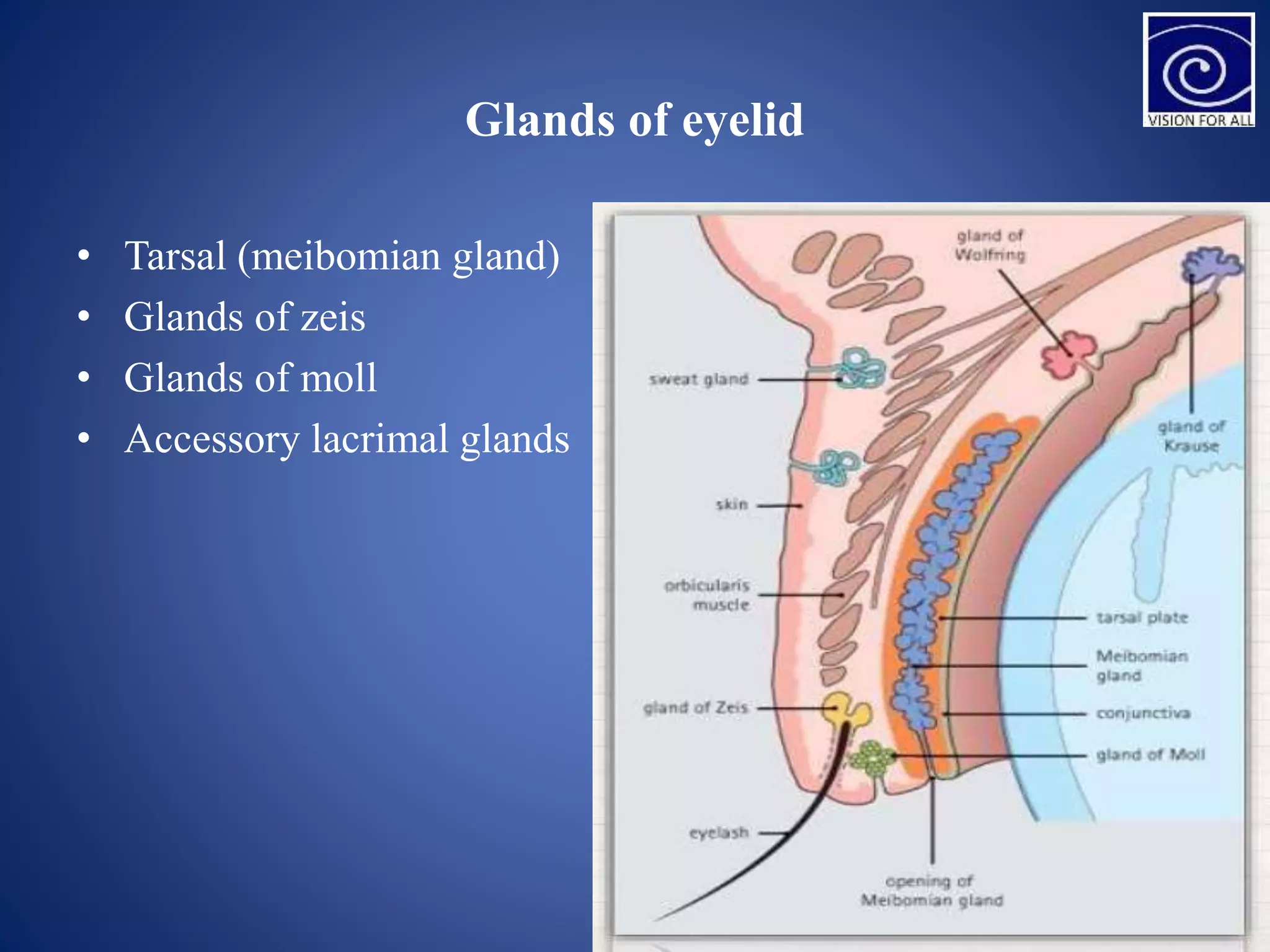
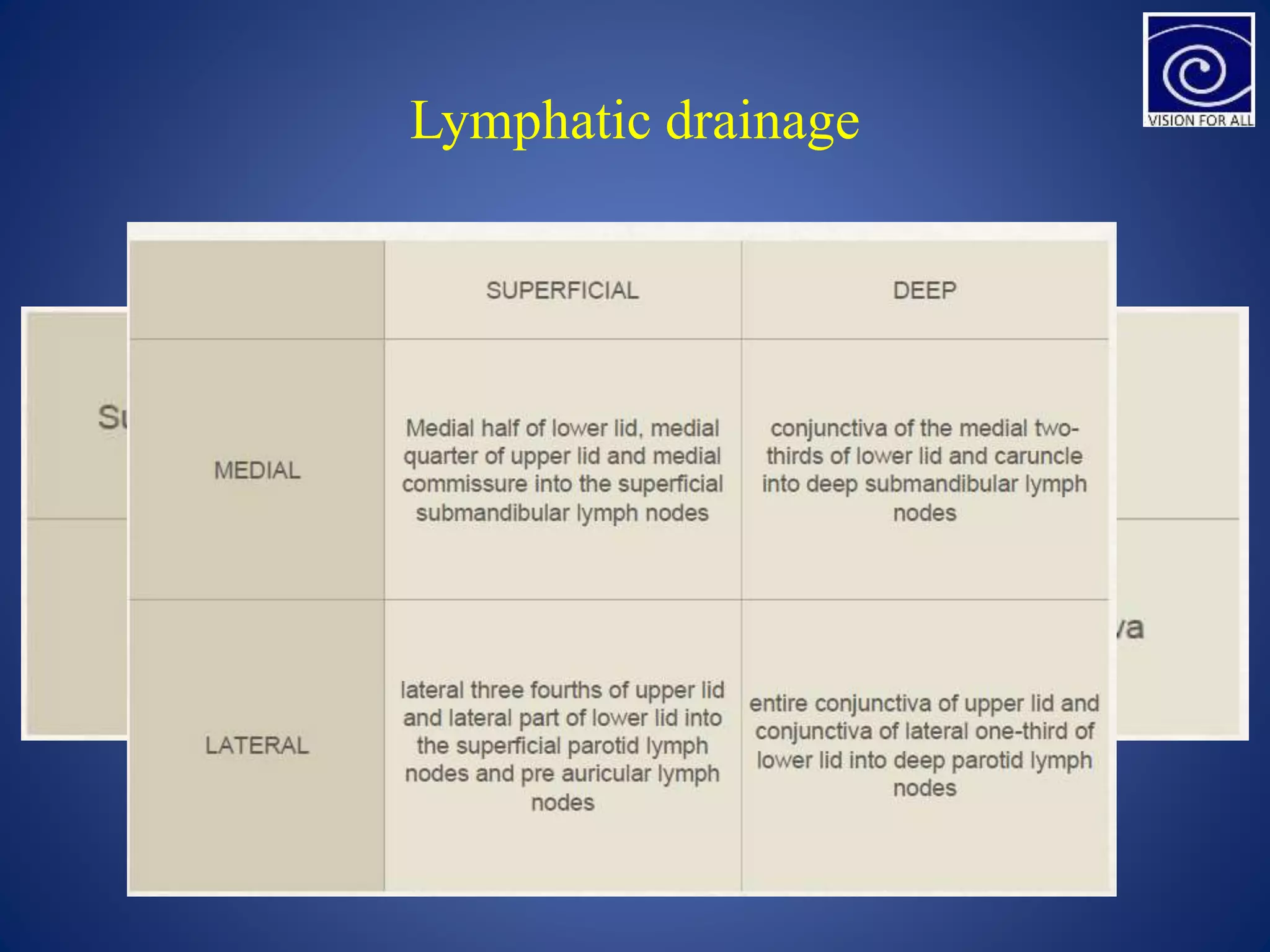
The document provides an overview of the anatomy of the eyelid. It describes the eyelid's gross anatomy including its extent, folds, margins, lashes and palpebral aperture. It details the layers that make up the eyelid including skin, muscles such as the orbicularis oculi and levator palpebrae superioris, and glands like the meibomian and moll glands. The arterial blood supply and lymphatic and nerve drainage of the eyelid are also summarized.