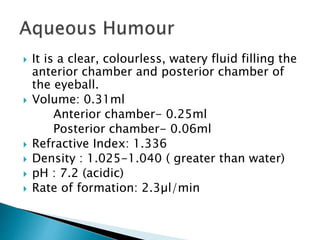
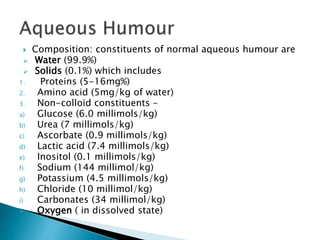
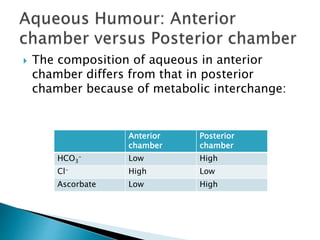
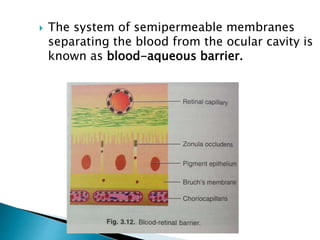
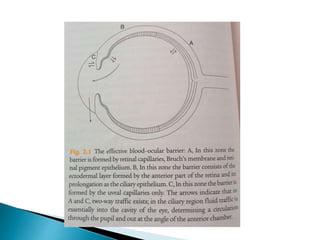
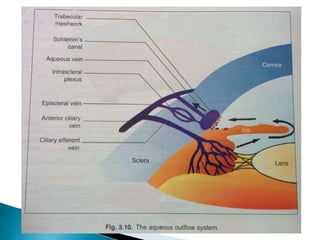
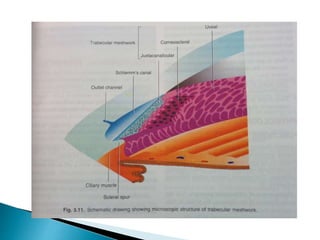
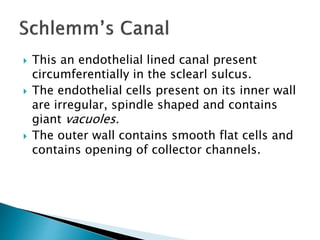
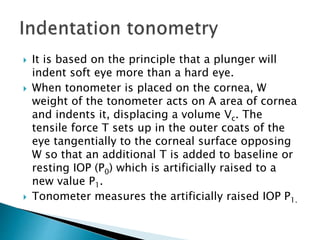
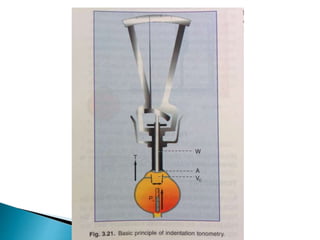
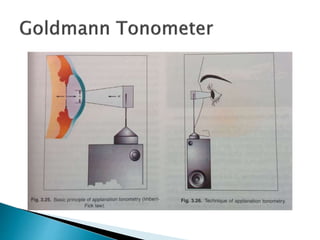
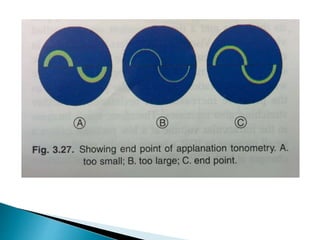
The document summarizes key details about aqueous humour, including its composition, production, circulation and role in maintaining intraocular pressure (IOP). Aqueous humour is produced by ultrafiltration and secretion within the ciliary processes. It flows from the posterior to anterior chamber through the pupil. It is drained out of the eye through the trabecular meshwork and uveoscleral outflow pathways. IOP is maintained through a dynamic equilibrium between aqueous production and outflow and can be measured indirectly using tonometry.