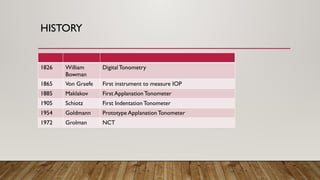
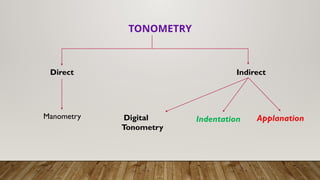
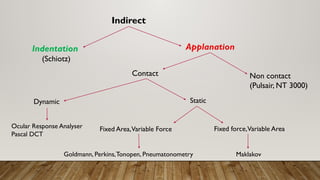
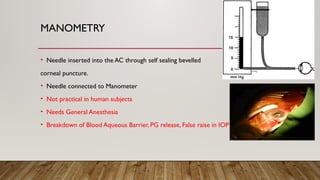
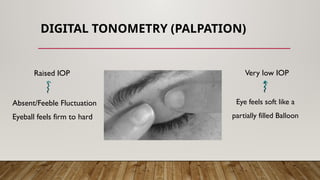
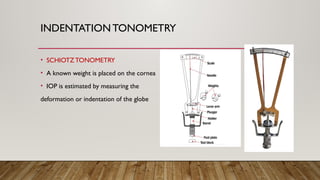
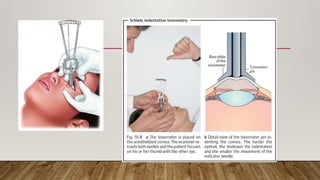
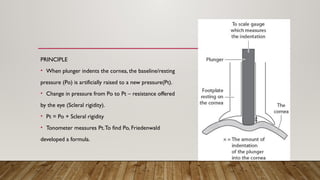
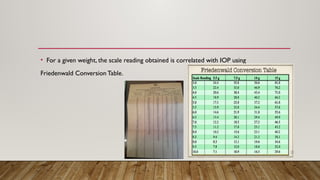
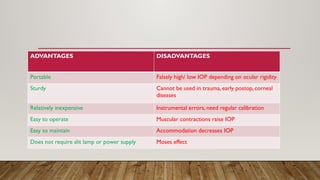
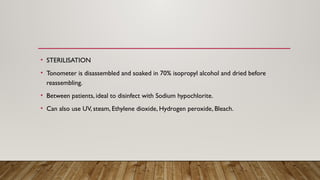
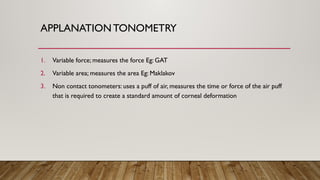
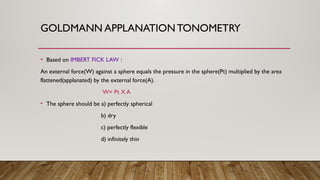
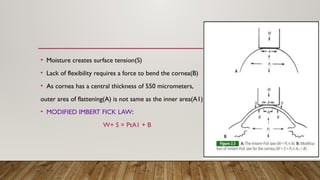
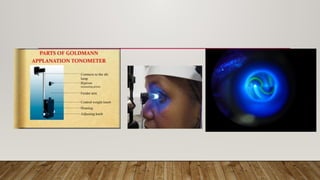
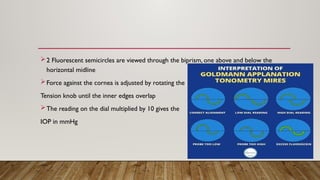
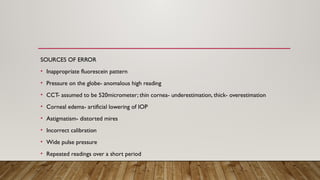
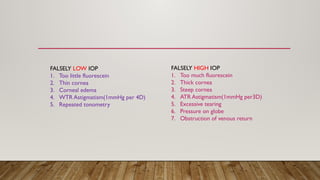
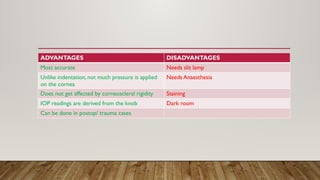
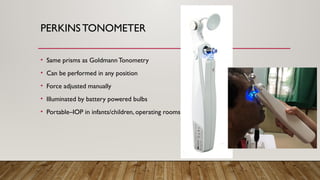
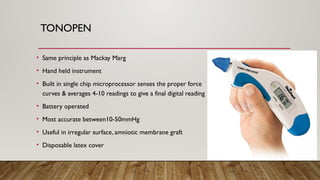
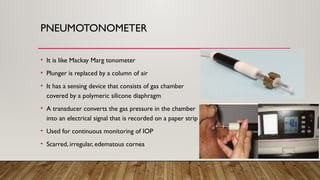
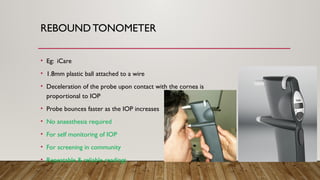
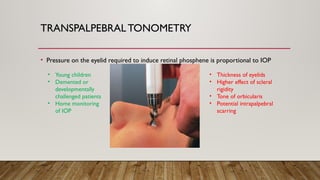
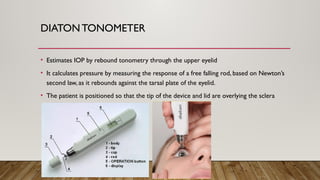
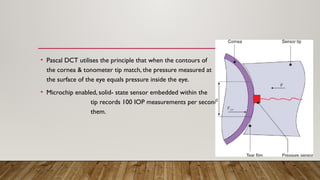
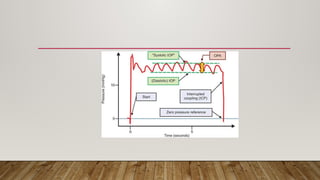
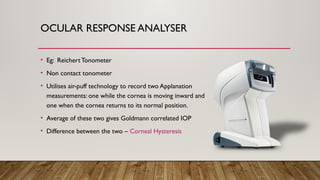
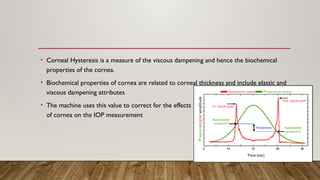
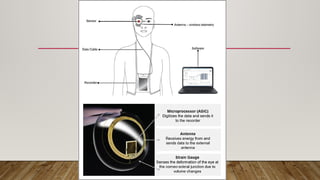
Tonometry is a procedure to measure intraocular pressure (IOP) using various techniques such as indentation, applanation, and non-contact methods. The document details the history, advantages, and limitations of different tonometry devices, including their operation, calibration, and specific applications for diverse corneal conditions. It also discusses potential sources of error and the importance of disinfection between uses to ensure accurate and safe measurements.