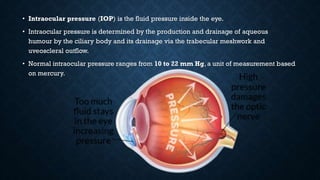
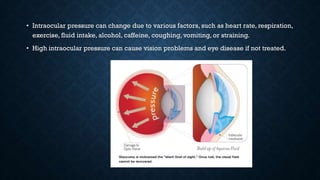
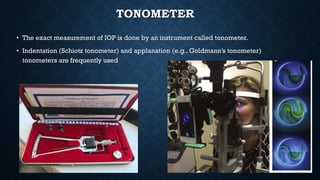
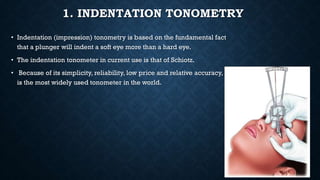
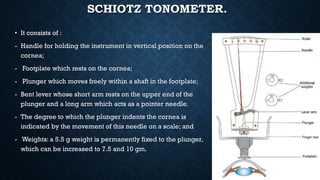
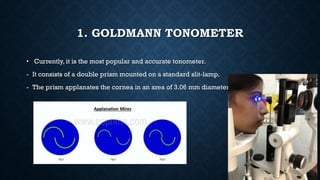
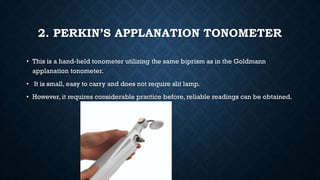
Intraocular pressure (IOP) is the fluid pressure inside the eye, which is normally between 10-22 mm Hg. IOP can be measured using indentation tonometry like the Schiotz tonometer or applanation tonometry like Goldmann tonometer. The Schiotz tonometer uses weighted plungers to indent the eye, while Goldmann tonometer uses two prisms to flatten a small area of the cornea to measure pressure. Other techniques include pneumatic tonometry and air puff tonometry. Accurately measuring IOP is important for diagnosing and managing glaucoma.