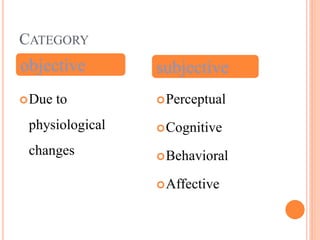
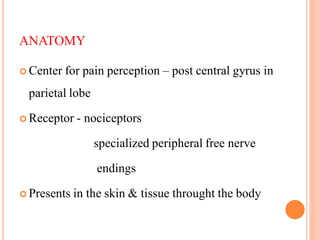
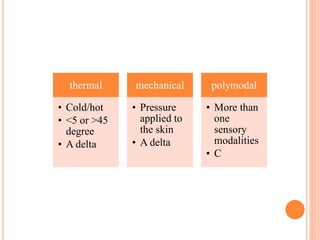
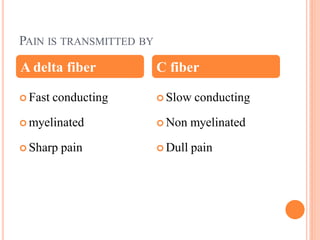
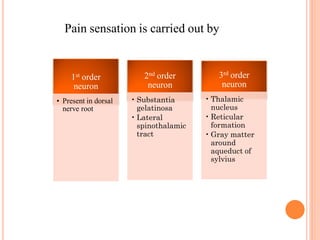
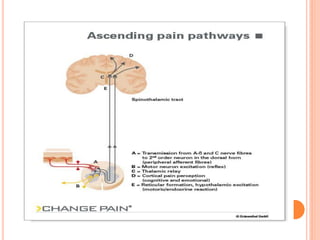
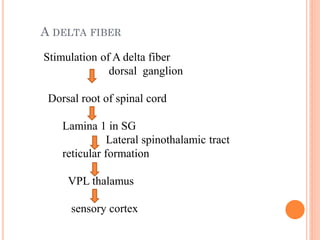
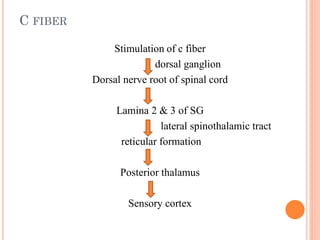
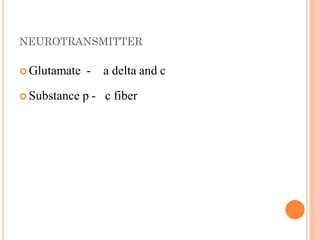
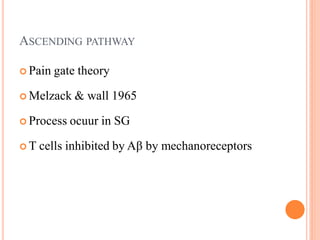
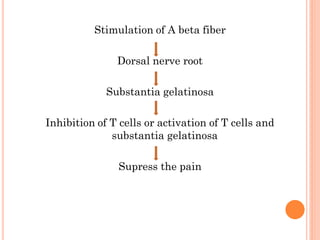
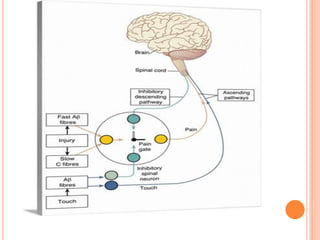
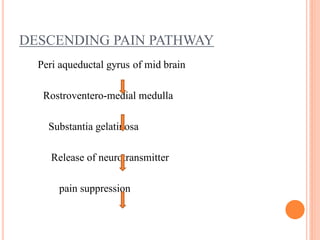
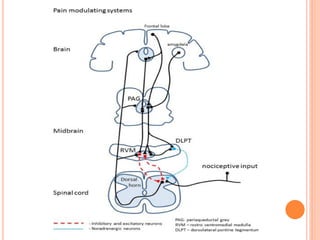
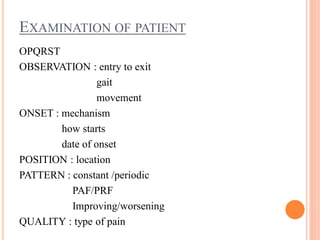
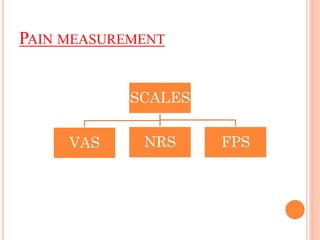
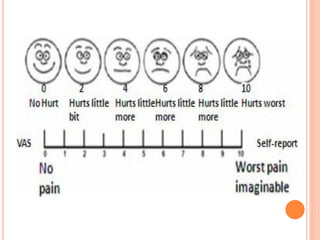
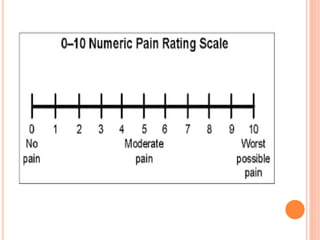
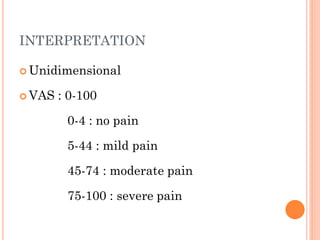
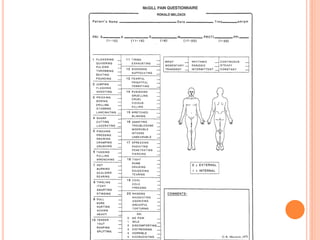
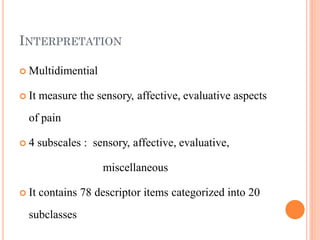
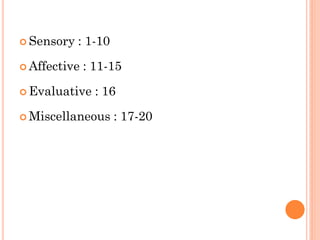
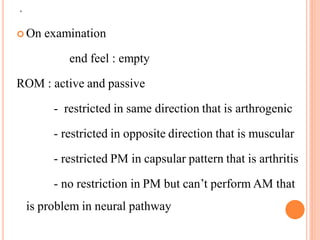
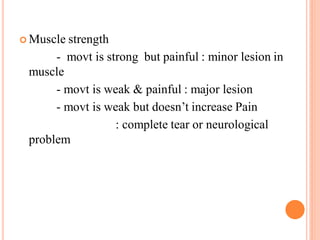
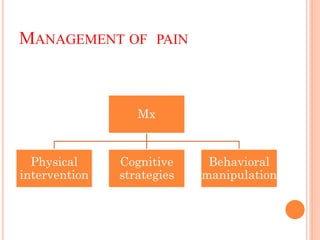
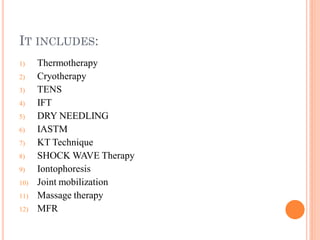
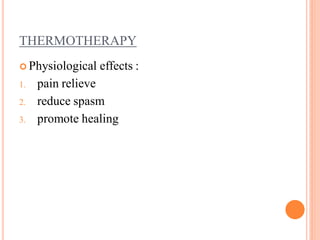
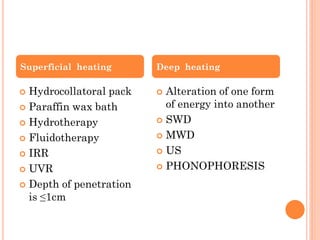
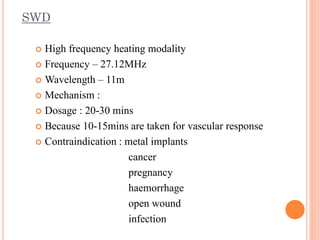
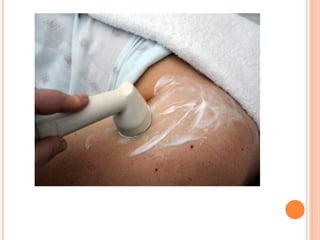
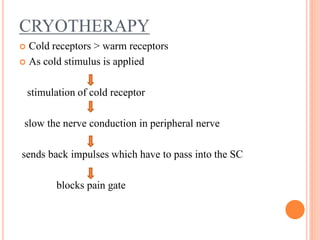
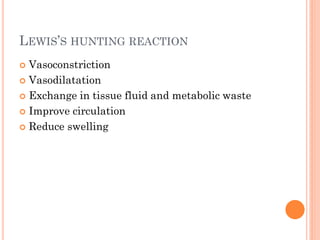
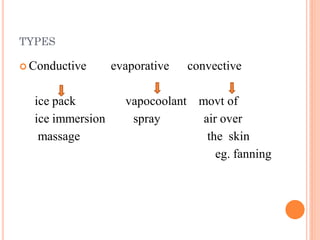
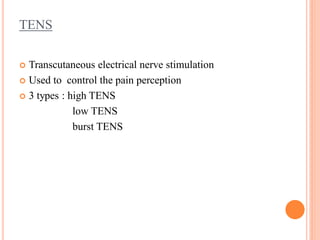
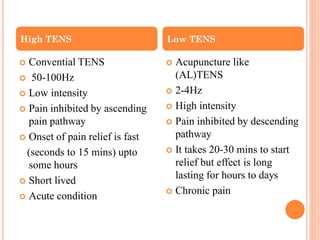
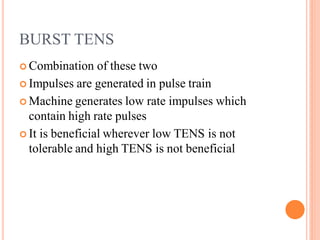
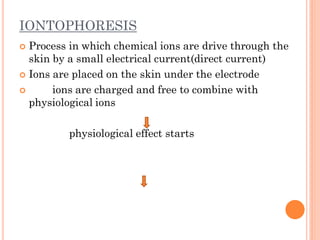
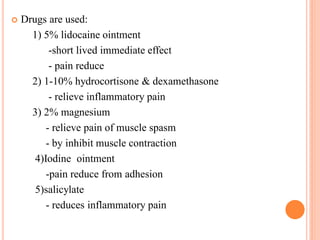
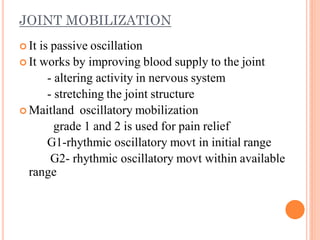
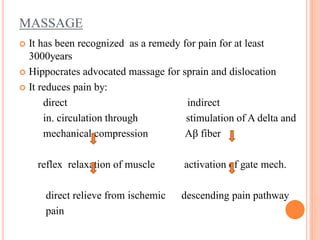
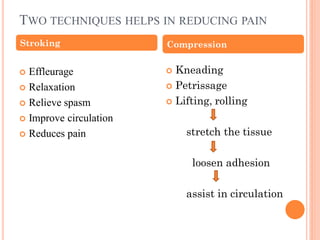
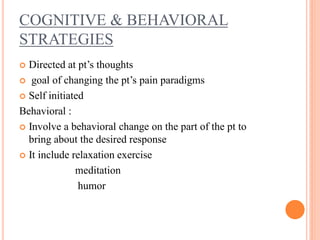
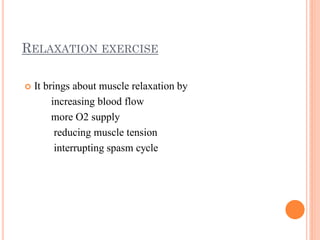
The document provides a comprehensive overview of pain, including its definitions, types (acute, chronic, referred, neuropathic), and mechanisms of pain perception and modulation. It discusses various assessment methods and treatment approaches, such as physical interventions, cognitive strategies, and behavioral manipulations, highlighting the importance of effectively managing pain. Detailed descriptions of assessment scales and specific treatment modalities, including thermotherapy, cryotherapy, and TENS, are also covered.