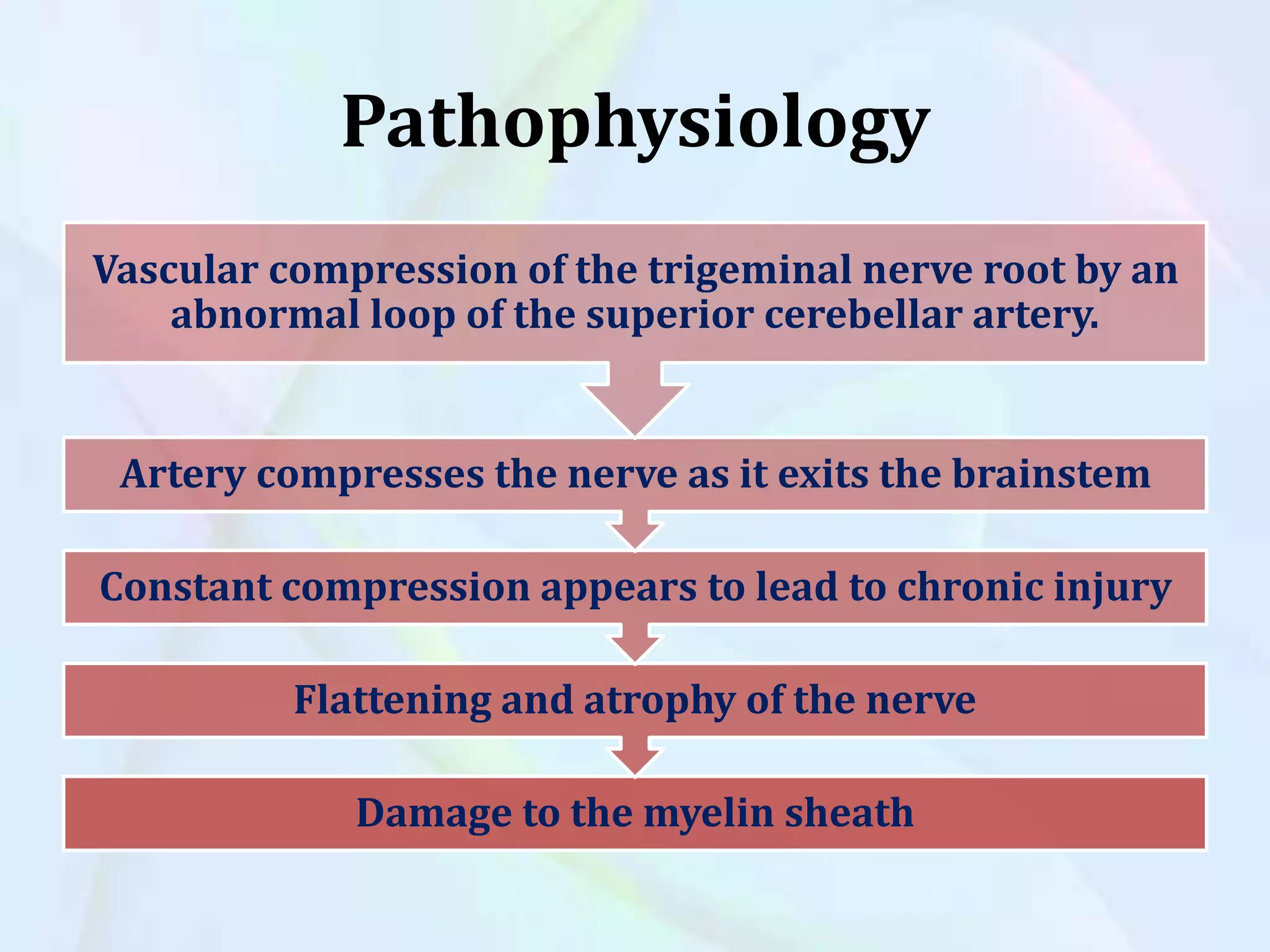
Cranial nerve disorders involve damage to the 12 pairs of cranial nerves, which are the peripheral nerves of the brain. Two common cranial nerve disorders are trigeminal neuralgia and Bell's palsy. Trigeminal neuralgia causes sudden, severe facial pain and is often caused by compression of the trigeminal nerve by blood vessels. Bell's palsy results in temporary facial paralysis or weakness on one side of the face, usually from herpes zoster infection or other causes that damage the facial nerve. Both disorders are typically diagnosed based on symptoms and treated initially with medications, nerve blocks, or in severe cases surgery to decompress nerves.