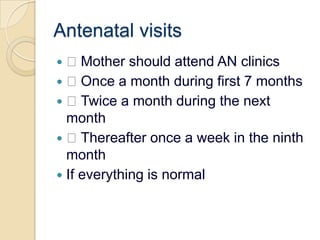
The document provides an introduction to maternal and child health. It notes that in developing countries, women of childbearing age and children under 15 make up 59% of the population and are vulnerable groups. Maternal and child mortality rates vary widely between countries. Mother and child health services have increasingly been integrated and provided as a package of essential primary healthcare. The document outlines various aspects of maternal and child health including antenatal care, maternal and infant health stages, and objectives and services provided during the antenatal period.