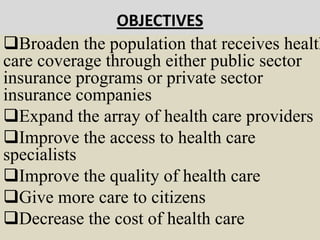
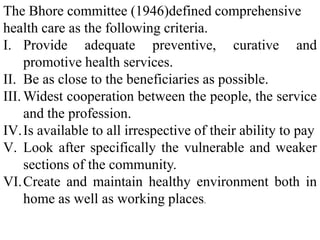
The document discusses health care reforms and the evolution of health care systems. It covers objectives of health care reforms such as expanding coverage and access to care. A major goal is providing better health care protection for more people at lower cost. Issues discussed include unequal distribution of health care resources between rural and urban areas, difficulties accessing care due to geographic, socioeconomic and gender factors, and how economic inequality affects health outcomes. The growth of the private health care sector is also addressed as adding to social inequities in access to affordable, quality care.