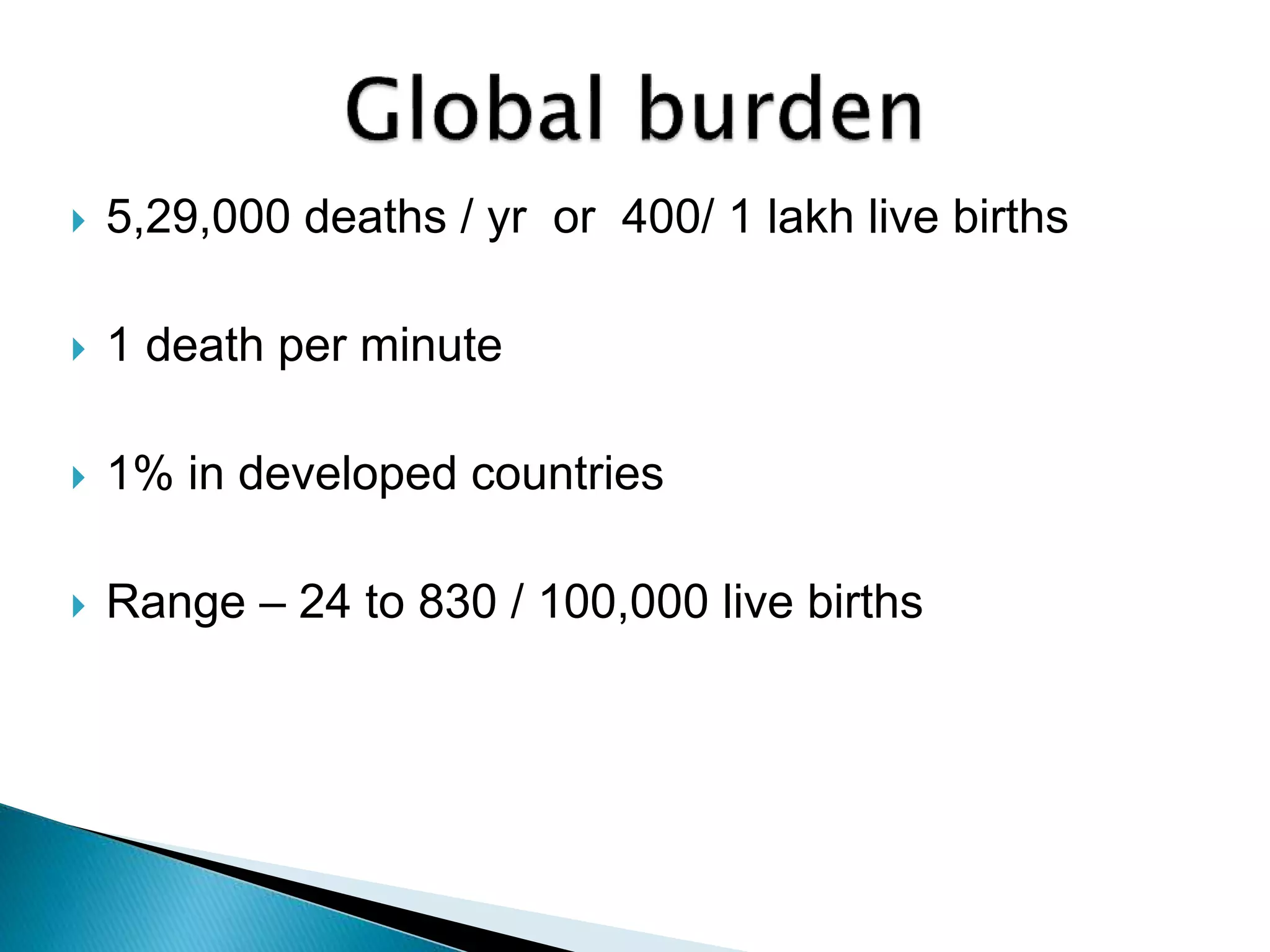
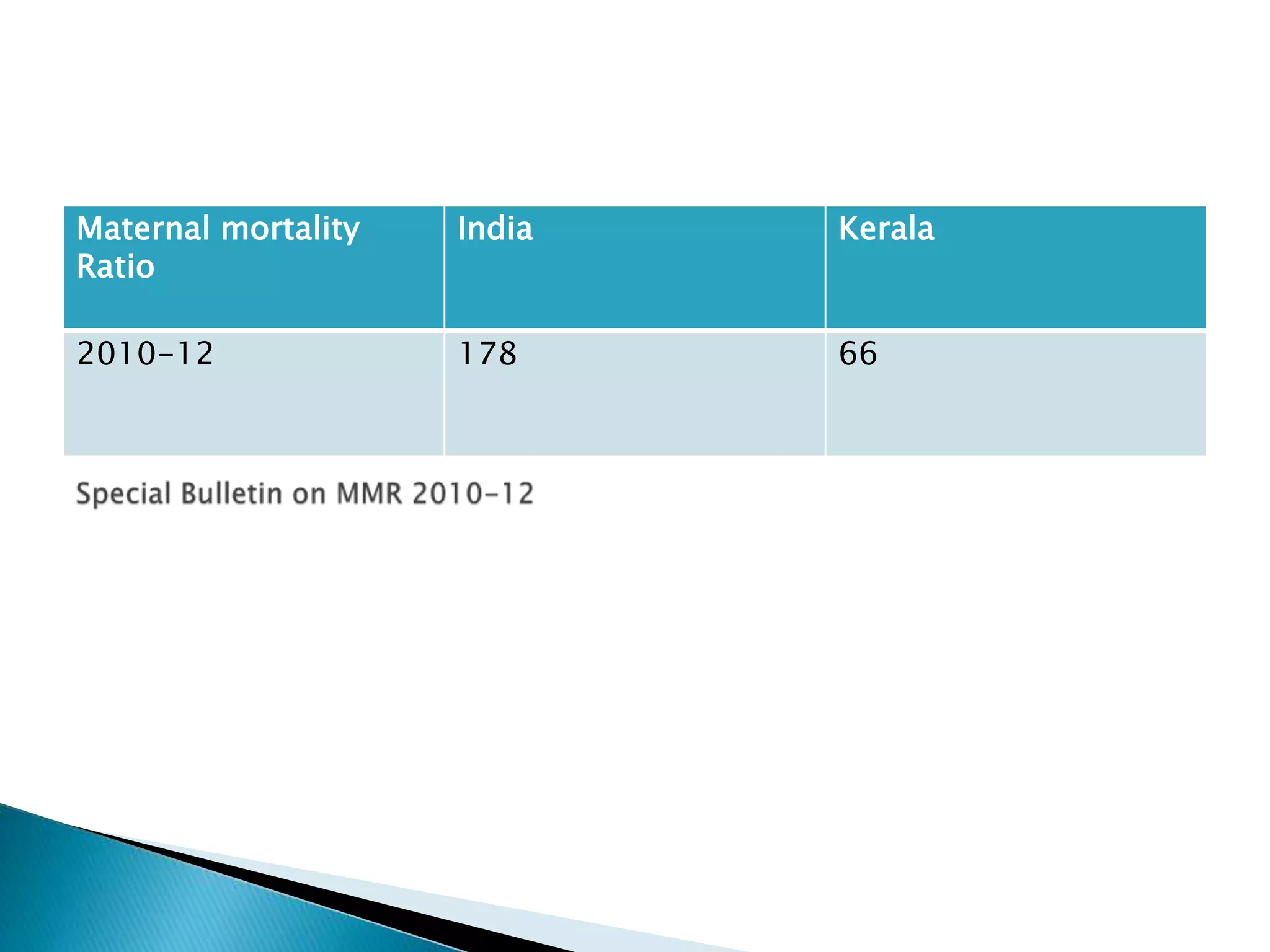
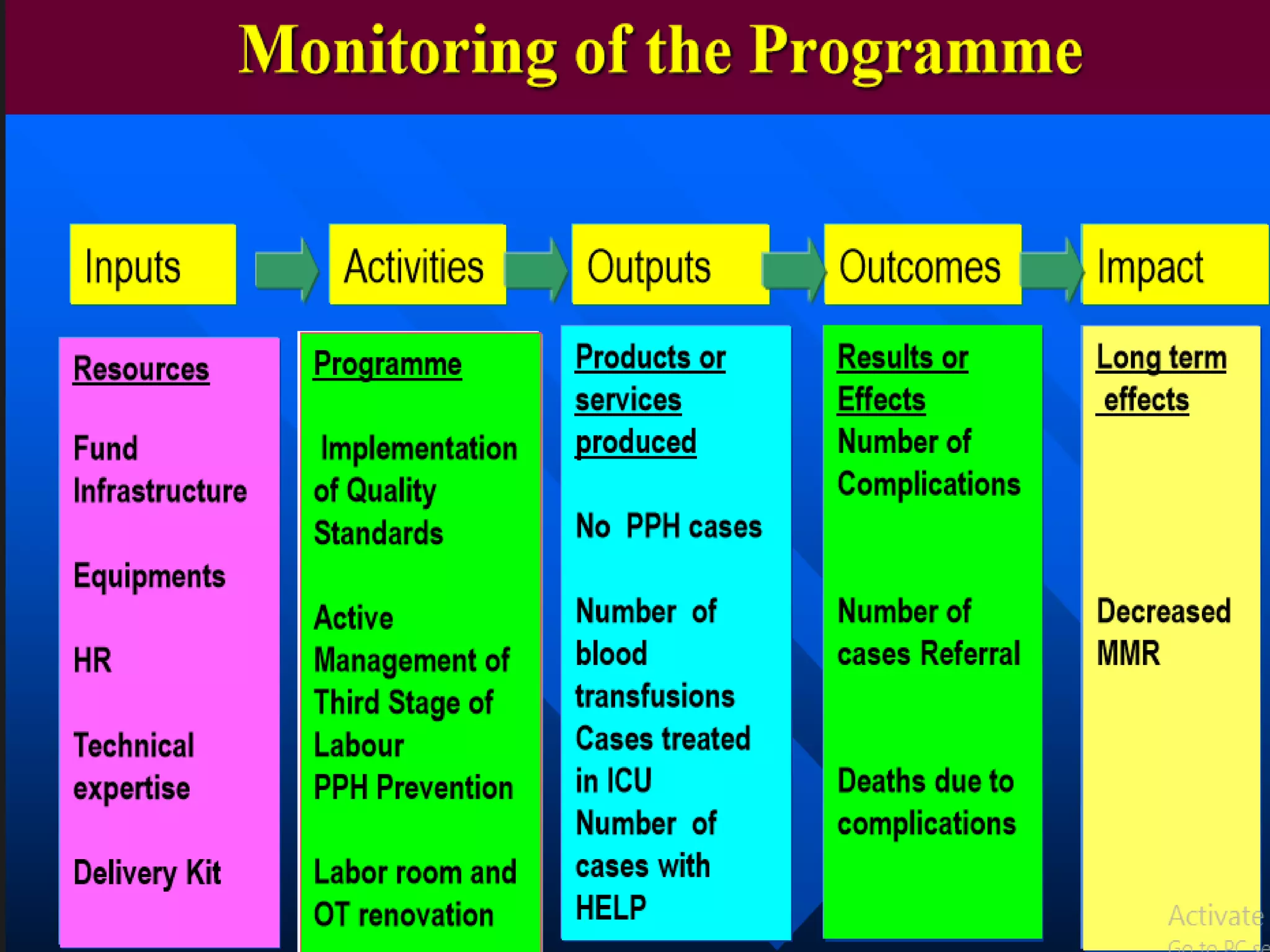
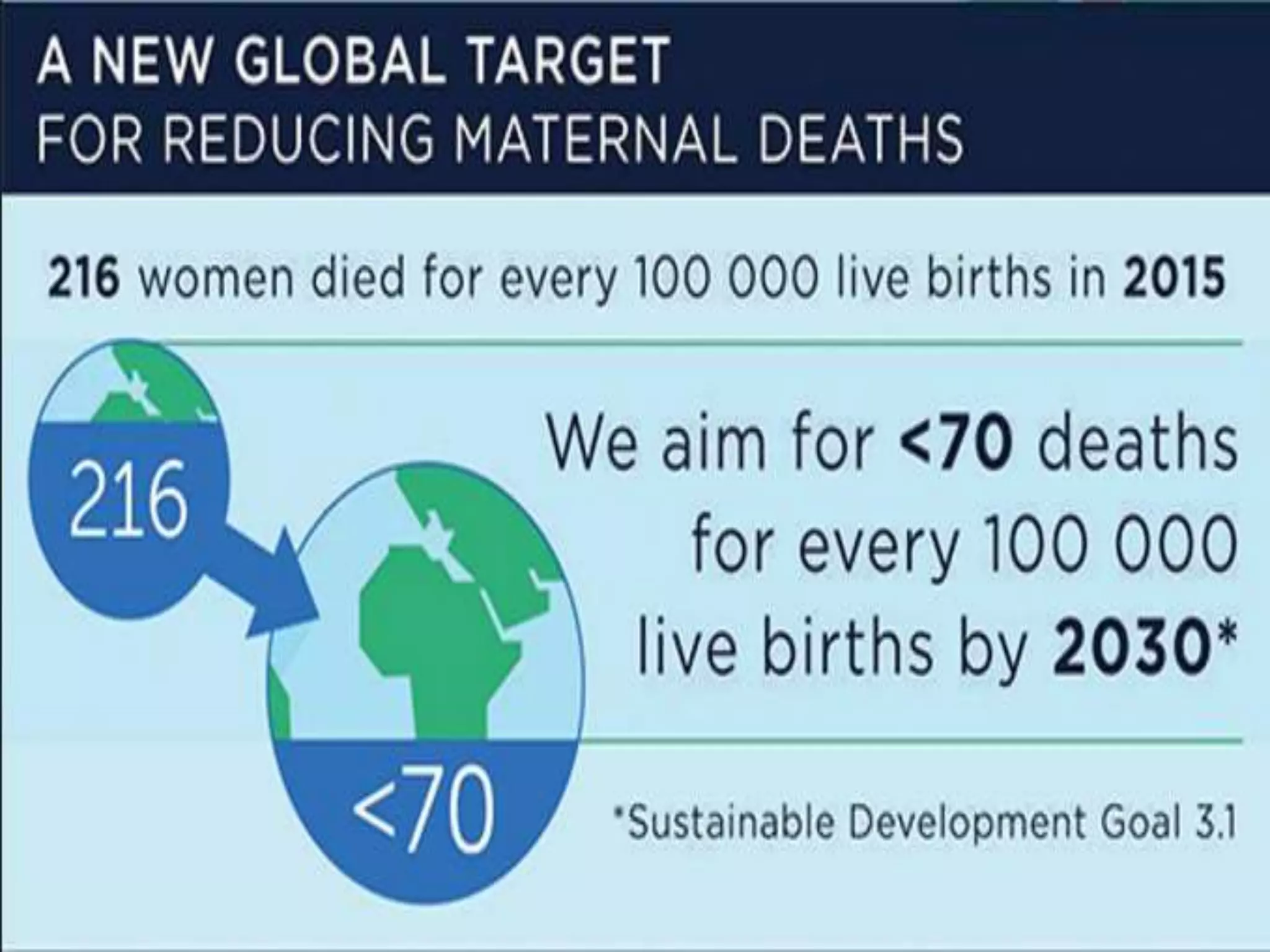
The document discusses maternal mortality, defining it as the death of a woman during or within 42 days of pregnancy termination from pregnancy-related causes. It provides global and Indian statistics on maternal mortality and approaches to measure it. The leading causes of maternal death worldwide and in India are discussed. Preventive measures to reduce maternal mortality are outlined, including antenatal care, skilled birth attendance, emergency obstetric care, and addressing social determinants. Initiatives taken in India like maternal death audits and clinical guidelines developed in Kerala are also summarized.