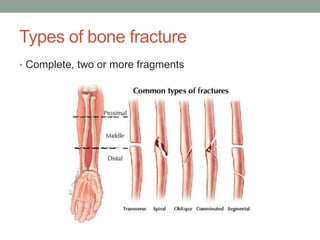
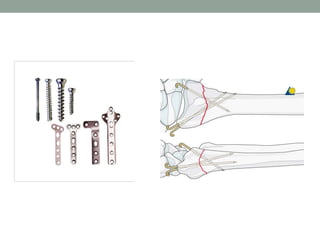
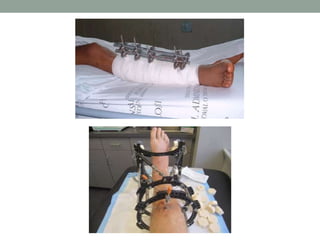
This document provides an introduction to bone fractures, including definitions, types, and treatment principles. It defines a bone fracture as a break in the structural continuity of bone. There are different types of fractures including complete, incomplete, stress, compression, and physeal fractures. The key principles of fracture treatment are to reduce the fracture by realigning the bone fragments, hold the fragments in place using various immobilization methods like casting or internal/external fixation, and exercise the area as appropriate for healing. Proper treatment helps the bone heal through either callus formation or direct healing of the bone edges.