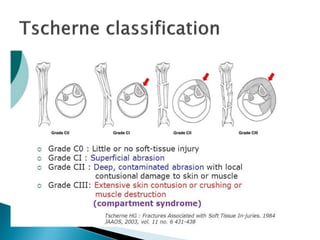
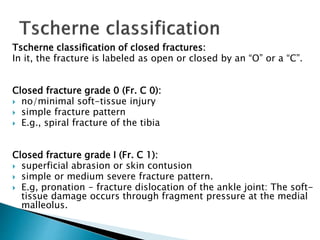
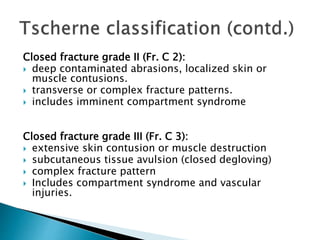
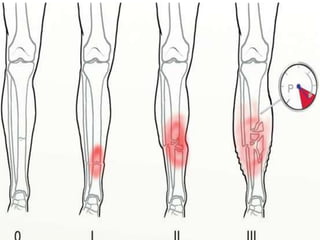
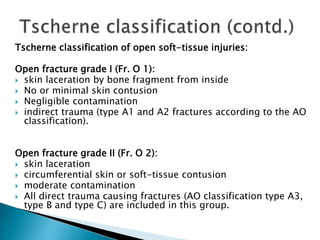
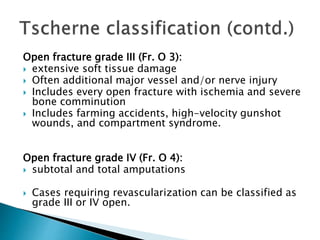
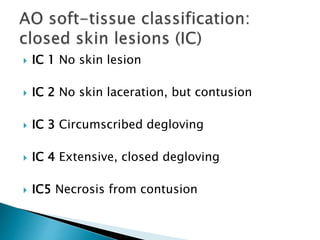
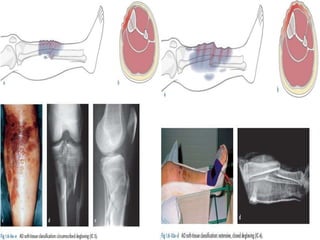
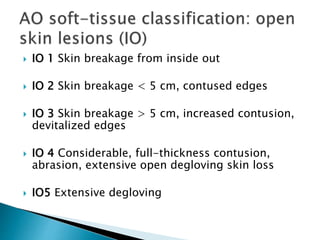
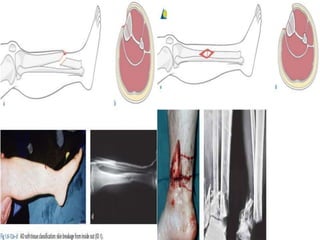
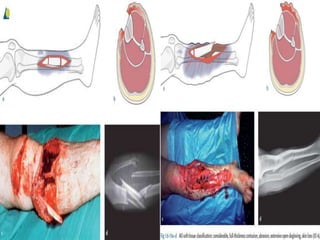
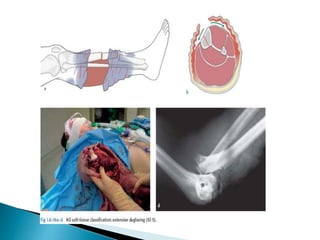
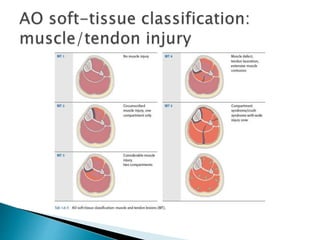
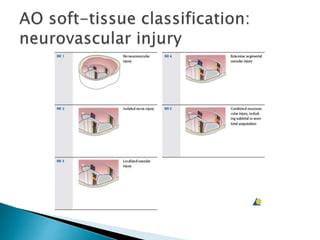
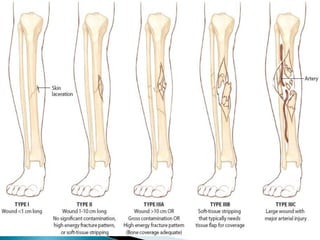
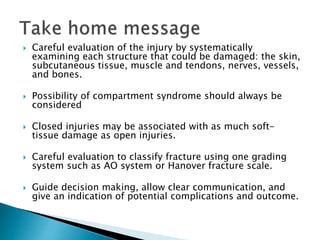
This document discusses the classification of soft tissue injuries associated with fractures. It describes several classification systems, including Tscherne, Gustilo-Anderson, and AO, that grade soft tissue injuries based on factors like wound size, contamination, and bone and muscle involvement. Proper classification of soft tissue injuries is important for determining fracture management and predicting healing to help standardize treatment protocols.

![SOFT TISSUE INJURY [Recovered].pptx](https://image.slidesharecdn.com/classificationofsofttissueinjuryrecovered-220424142623/85/SOFT-TISSUE-INJURY-Recovered-pptx-49-320.jpg)