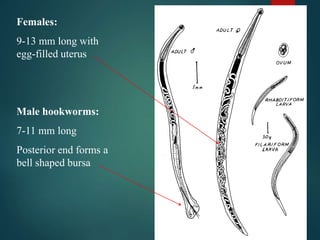
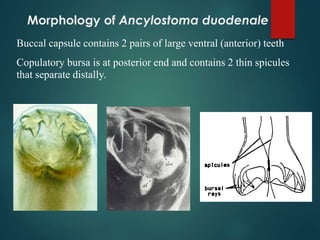
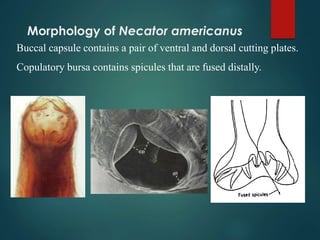
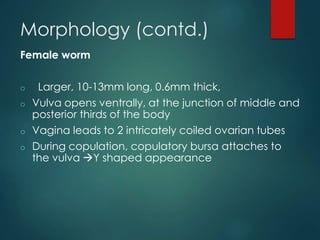
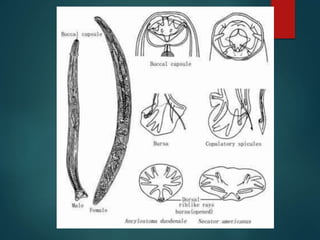
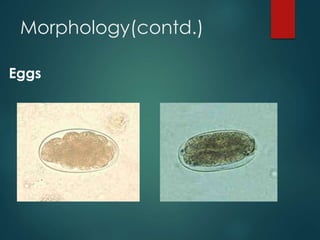
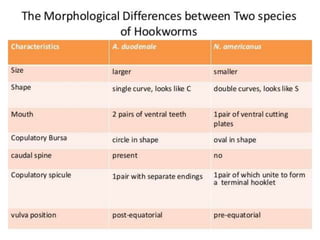
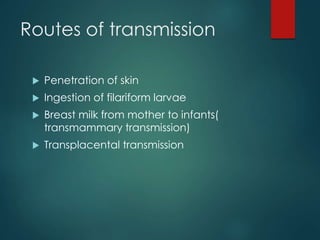
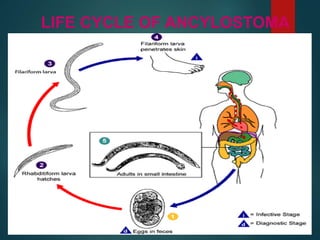
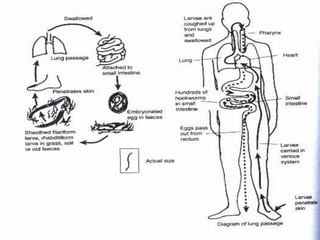
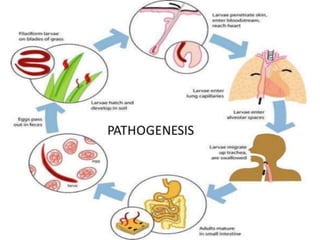
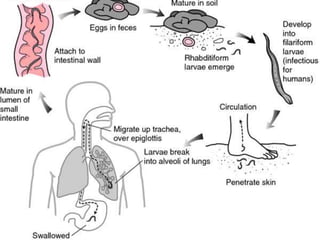
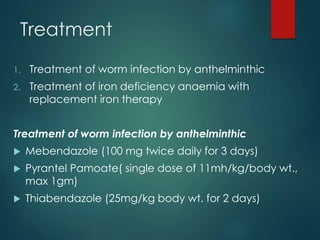
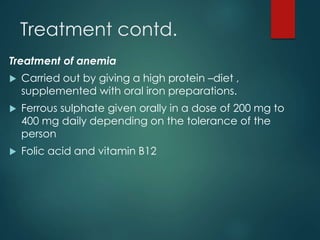
The document discusses Ancylostoma duodenale and Necator americanus, two species of hookworms, detailing their morphology, life cycle, transmission routes, and clinical manifestations. It emphasizes skin and respiratory symptoms, diagnosis challenges, and treatment options including anthelmintics and iron supplements. Prevention strategies involve sanitation, treatment of infected individuals, and health education.