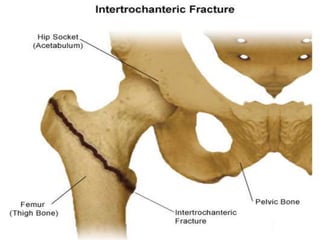
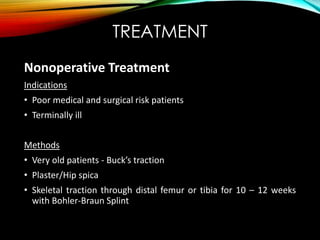
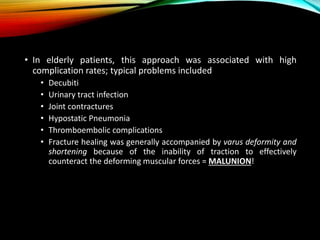
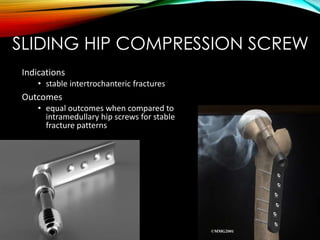
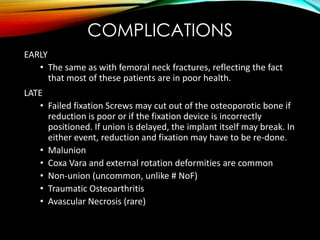
An intertrochanteric fracture occurs between the greater and lesser trochanters of the femur. It commonly results from a fall in elderly osteoporotic patients. While internal fixation is usually required, sliding hip screws are the most widely used implant due to their ability to stabilize both stable and unstable fracture patterns. Complications can include malunion, cut out of fixation screws, and failure of the implant.