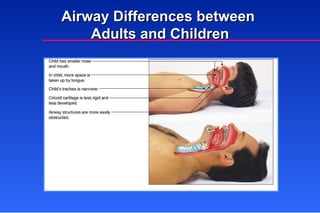
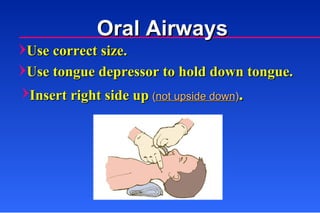
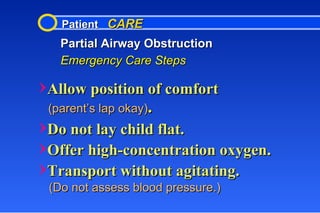
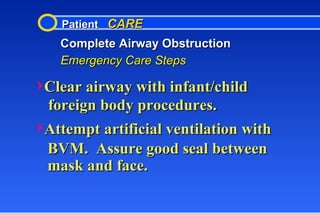
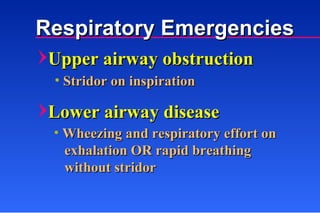
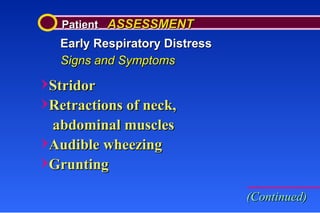
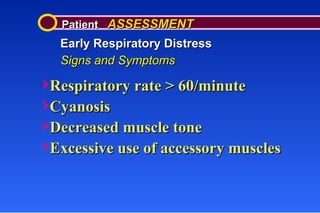
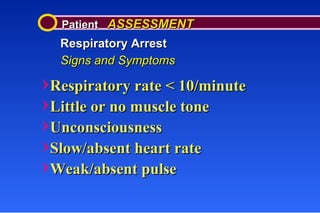
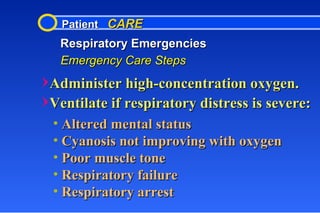
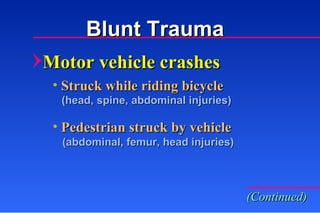
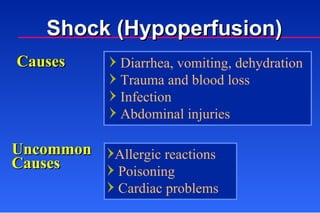
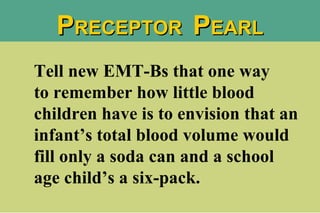
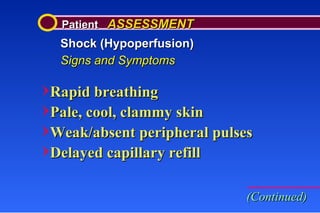
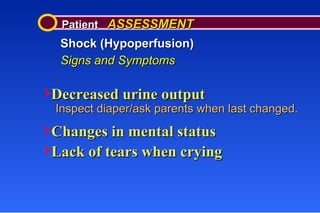
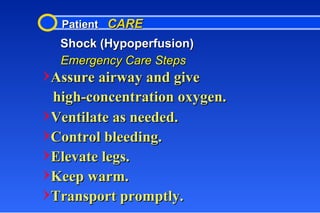
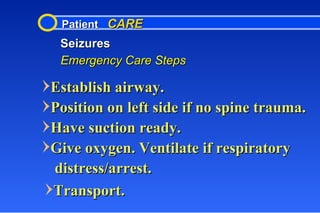
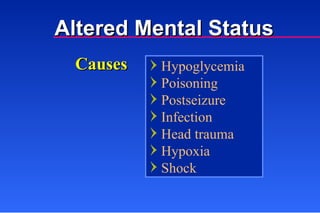
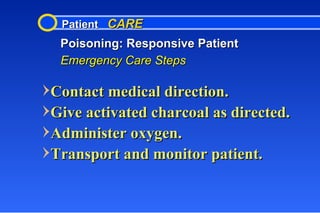
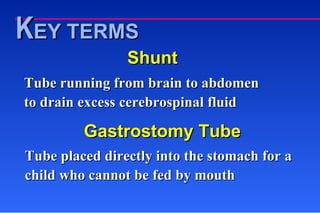
This document discusses pediatric medical emergencies, including respiratory emergencies, trauma, and shock. It provides assessment criteria and emergency care steps for various conditions in newborns, infants, toddlers, preschoolers, school-aged children and adolescents. Key points covered include assessing and managing partial and complete airway obstruction, respiratory distress, trauma injuries like head injuries, and shock. Emphasis is placed on maintaining the airway and providing oxygen in respiratory emergencies.