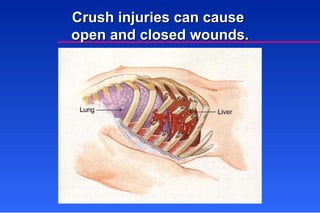
This document summarizes treatment for various soft tissue injuries including open and closed wounds, amputations, impaled objects, neck wounds, chest injuries, and burns. It describes assessing the injuries, providing emergency care such as controlling bleeding and preventing infection, dressing wounds, and guidelines for transporting patients.