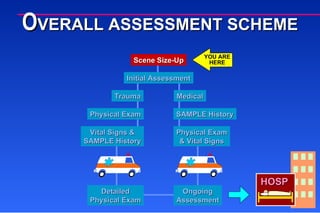
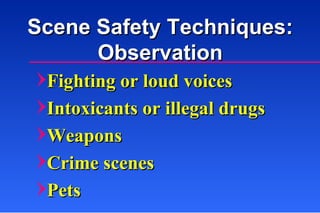
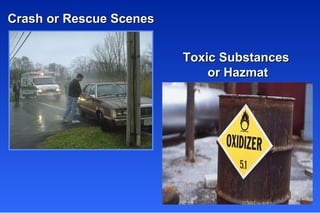
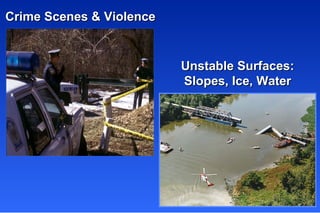
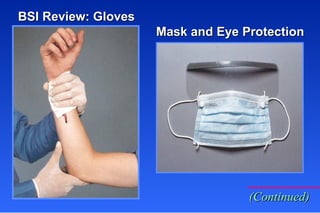
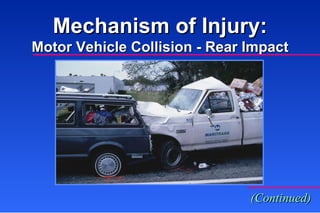
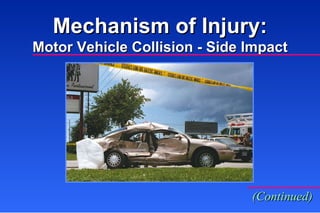
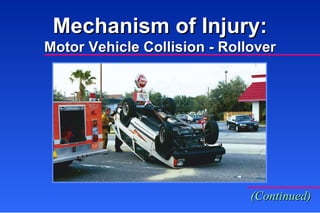
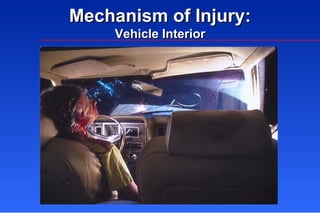
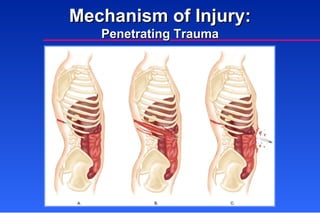
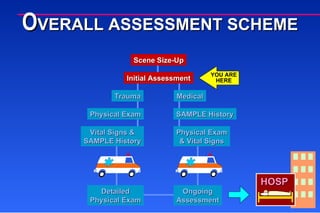
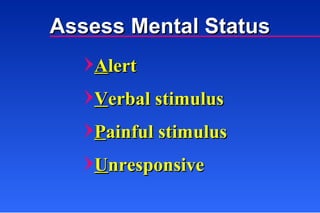
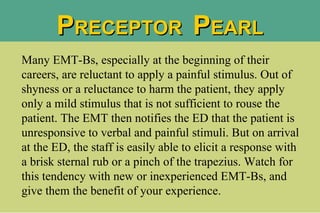
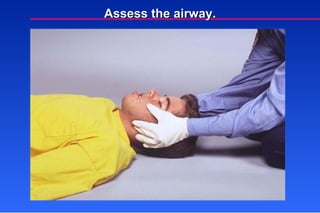
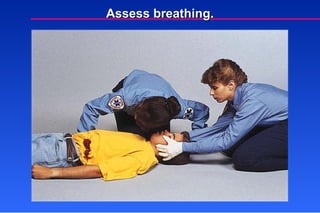
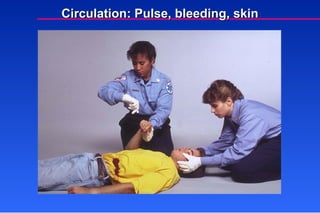
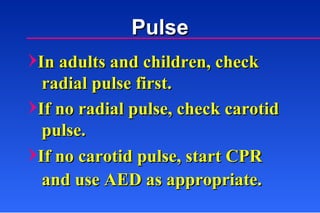
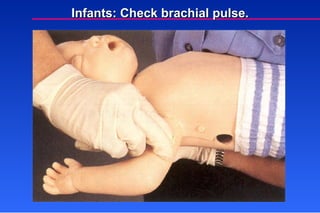
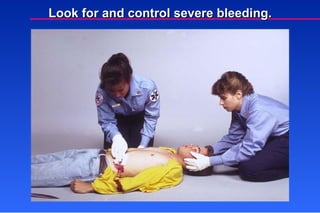
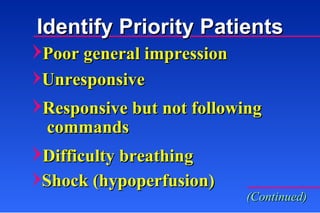
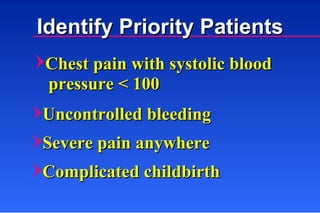
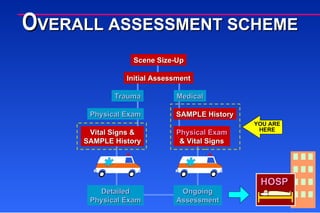
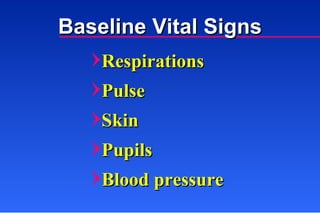
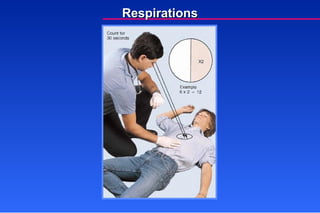
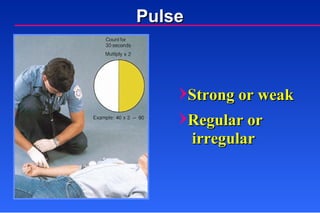
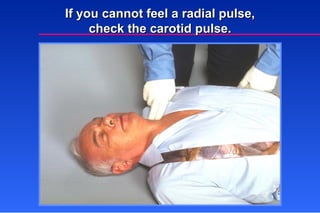
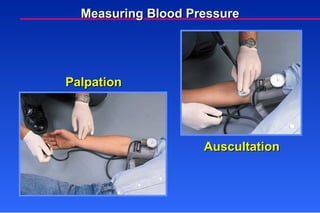
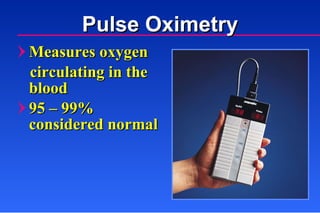
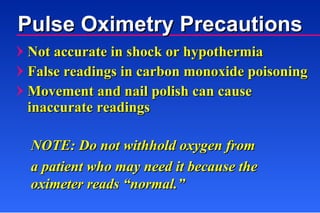
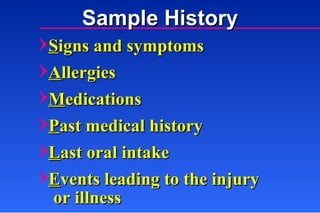
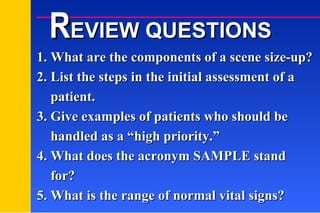
The document discusses the components of conducting a scene size-up and initial patient assessment, including scene safety, mechanism of injury, primary and secondary surveys, identifying priority patients, taking vital signs, and obtaining a SAMPLE history. Key steps include assessing the scene for safety, airway, breathing, circulation, mental status, and gathering patient information using the SAMPLE format of Signs/Symptoms, Allergies, Medications, Past medical history, Last oral intake, and Events leading to the current situation.