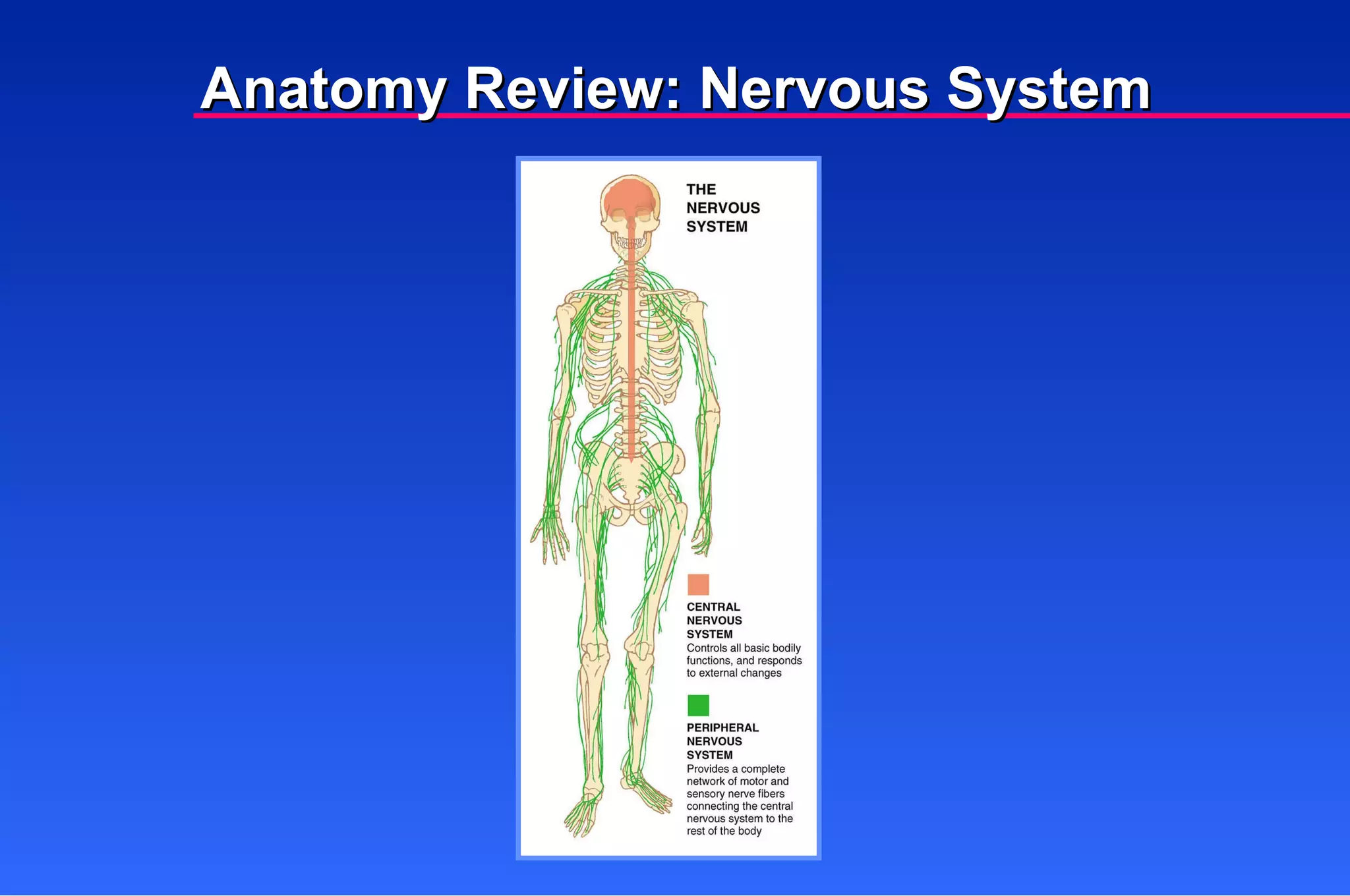
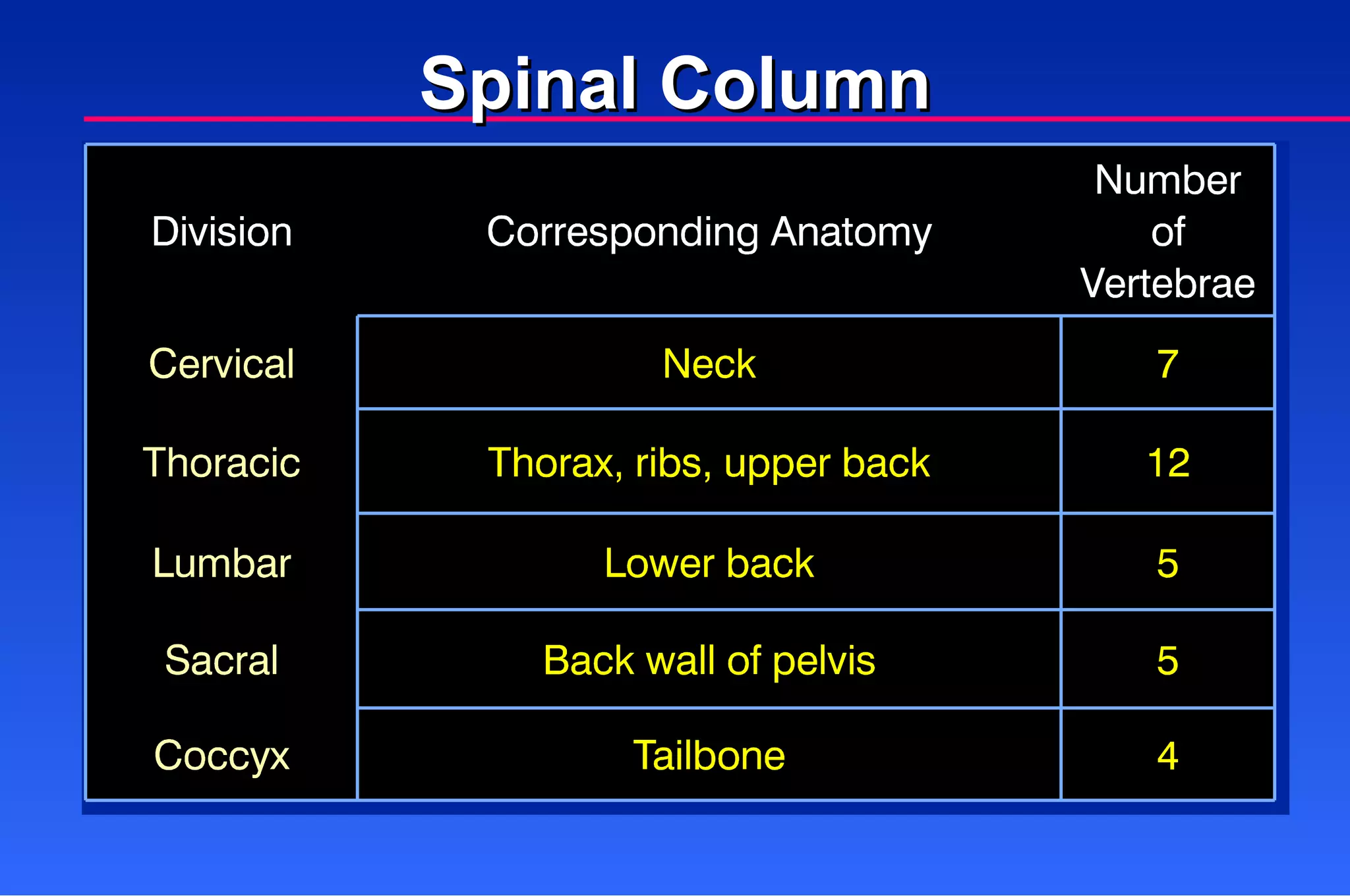
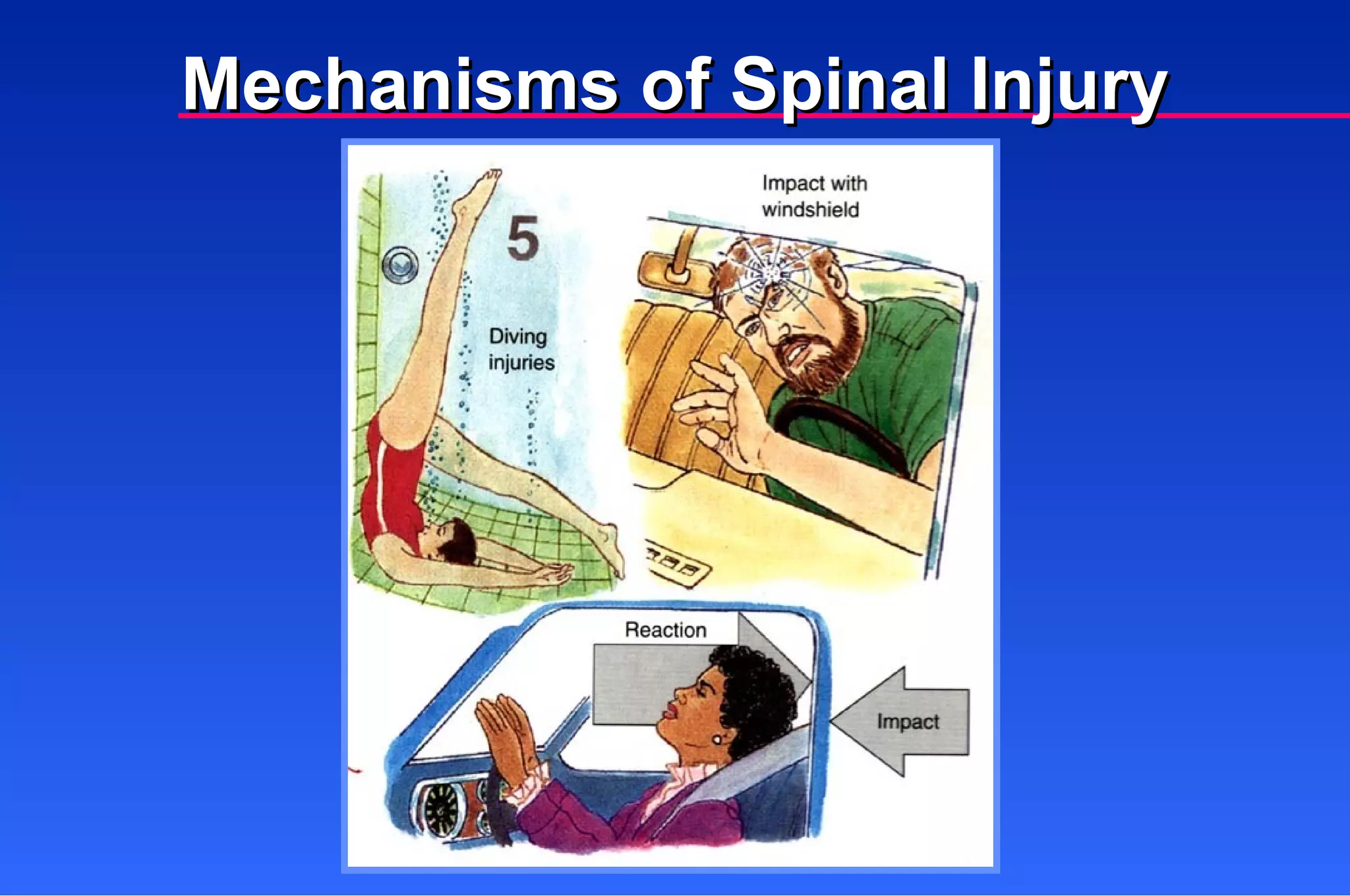
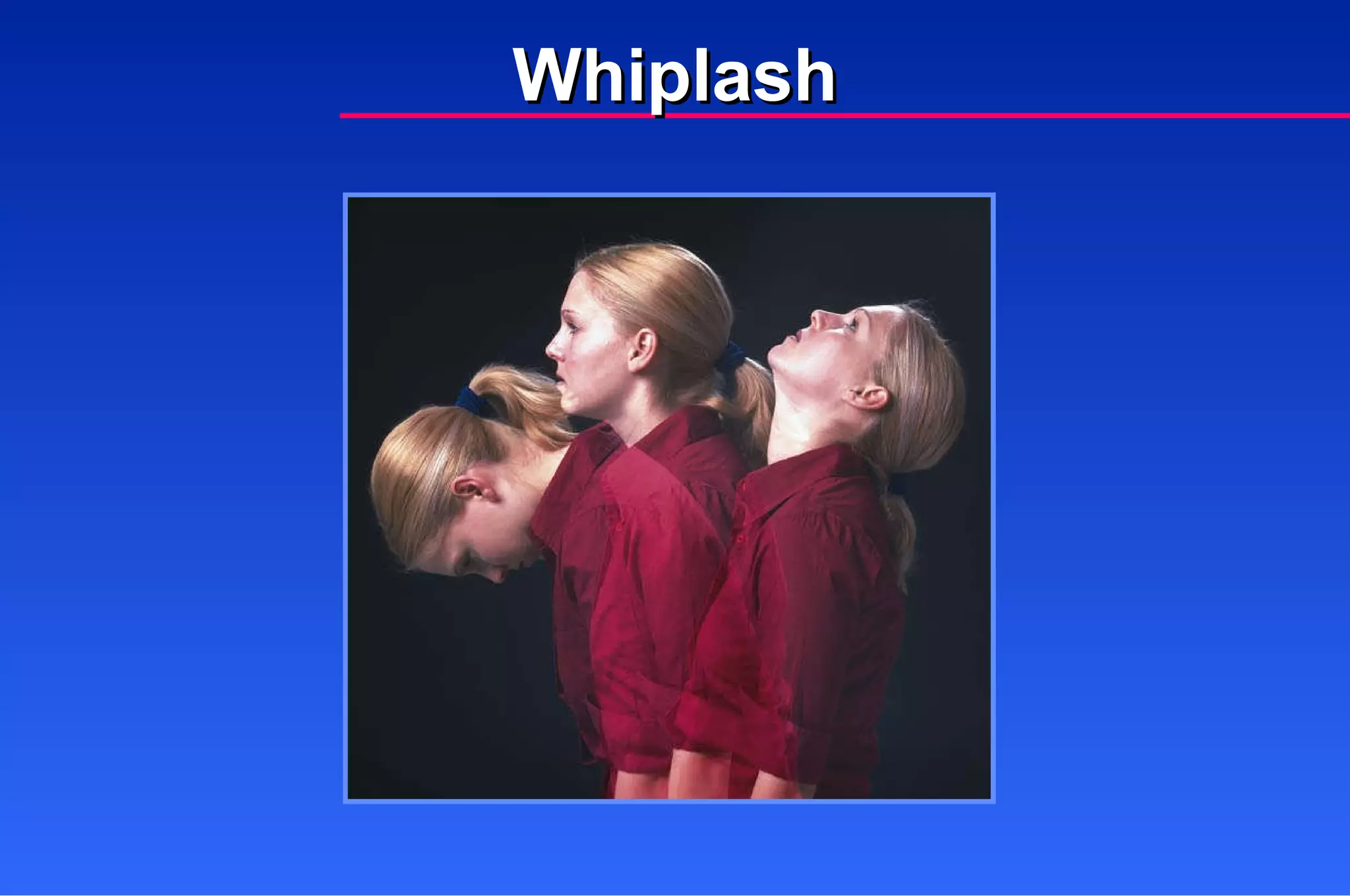
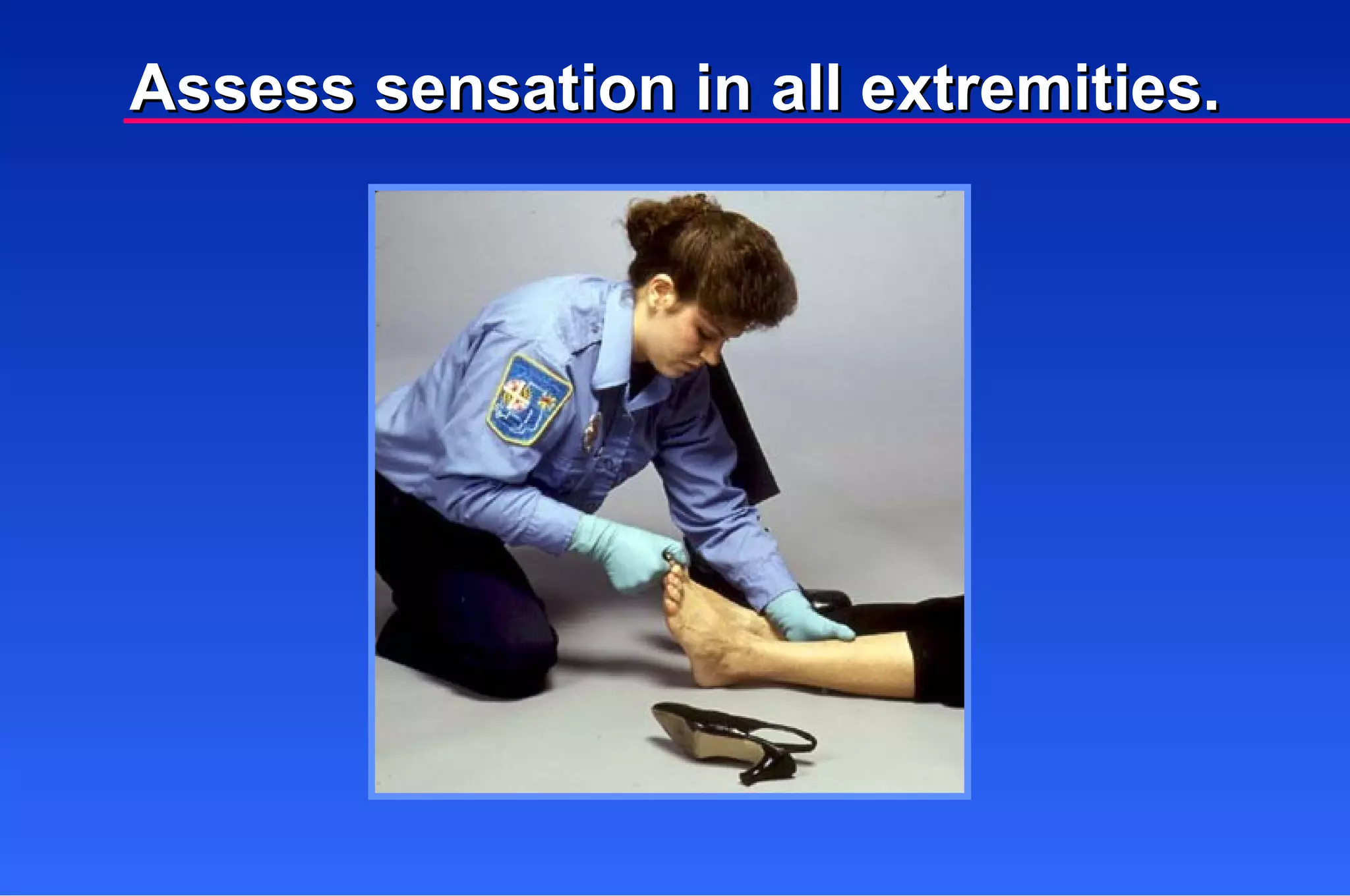
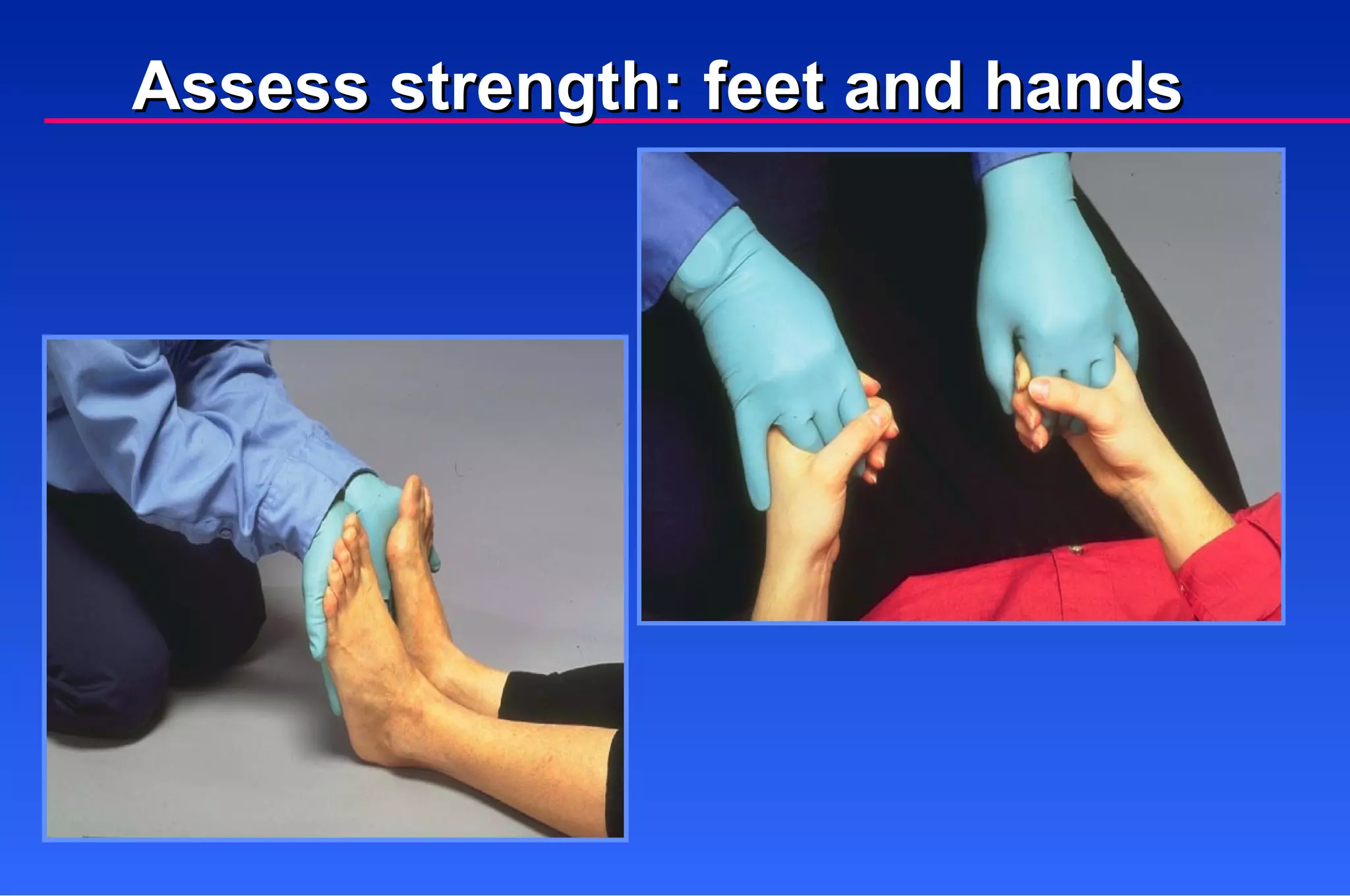
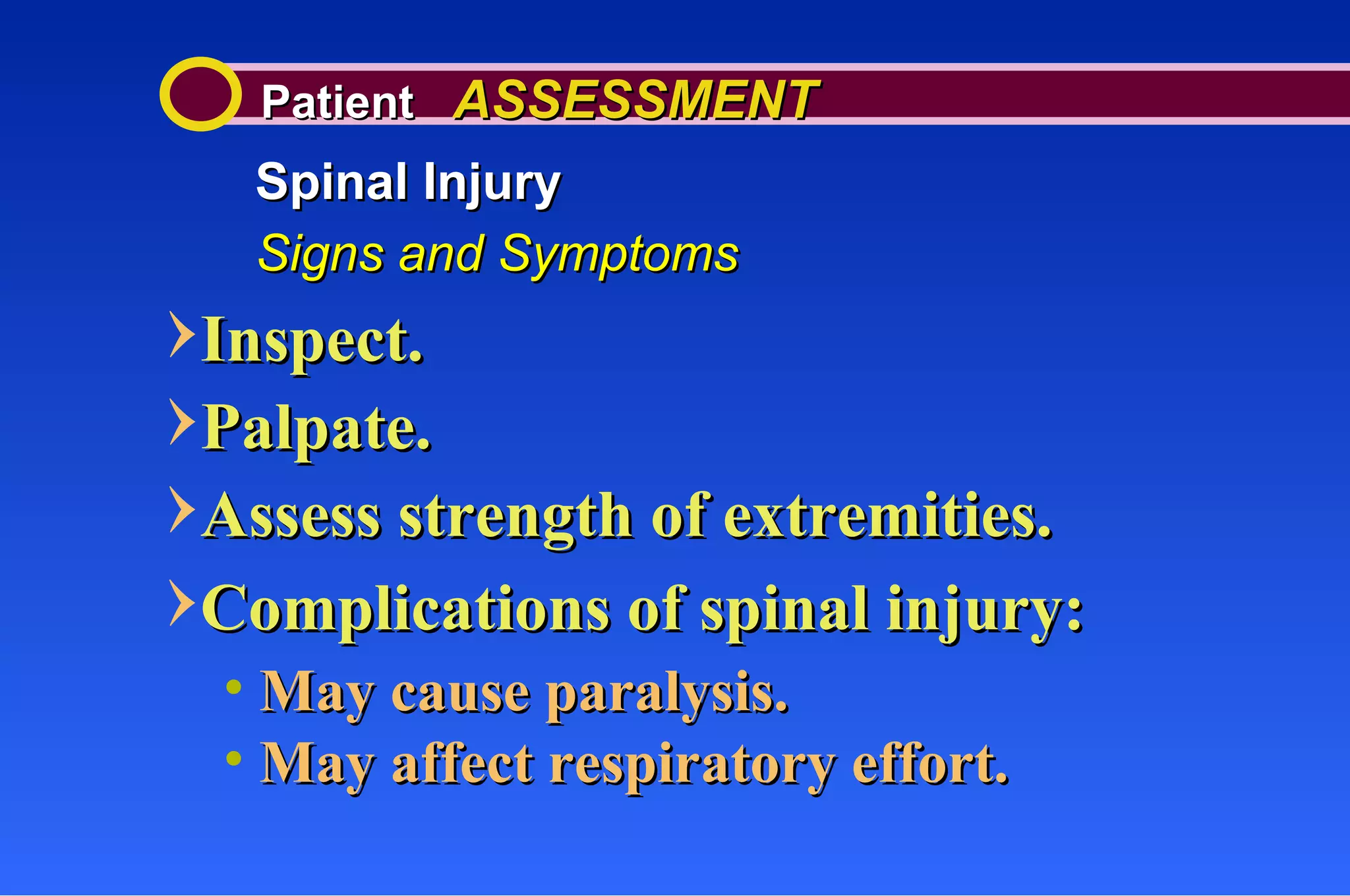
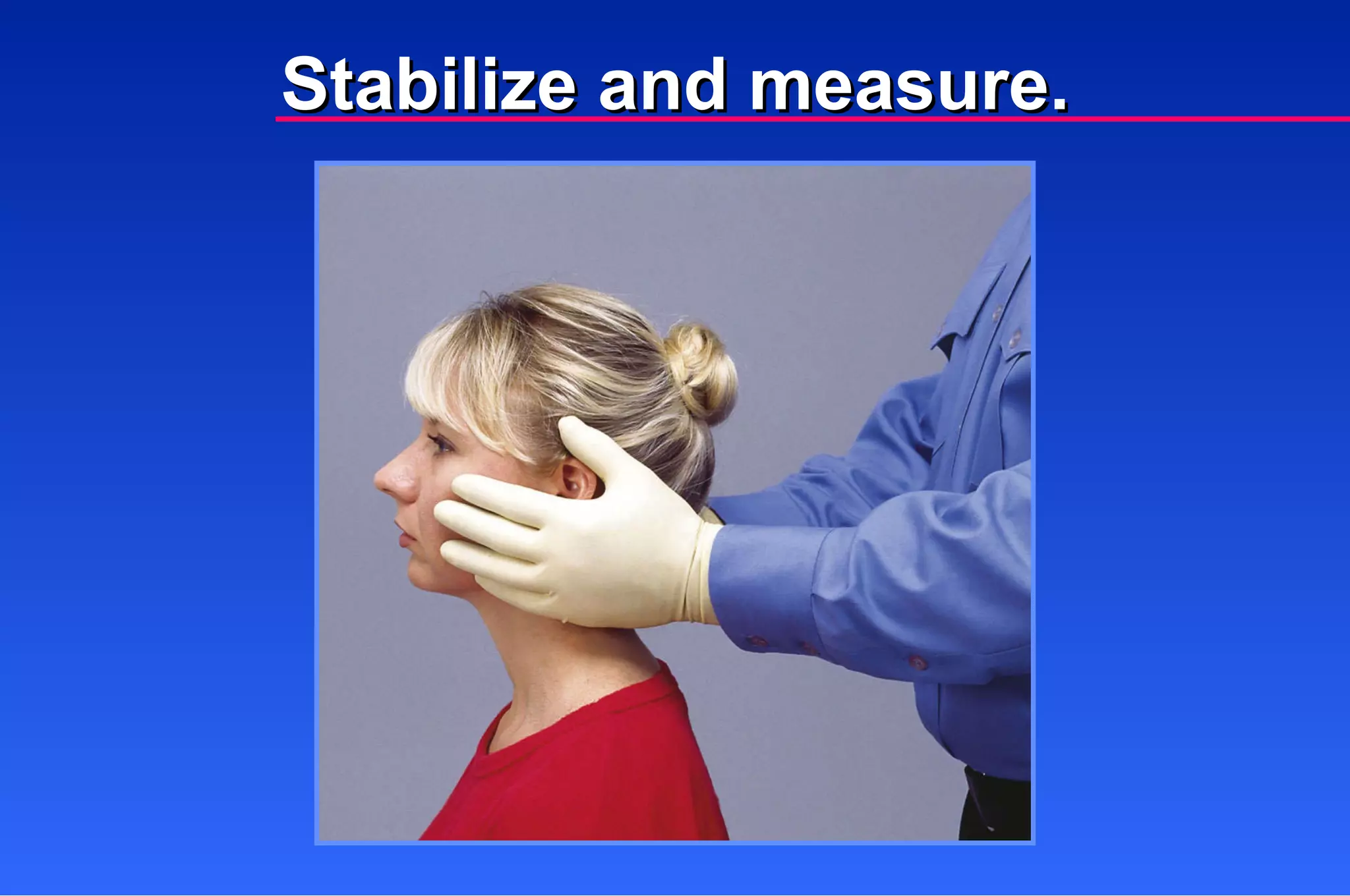
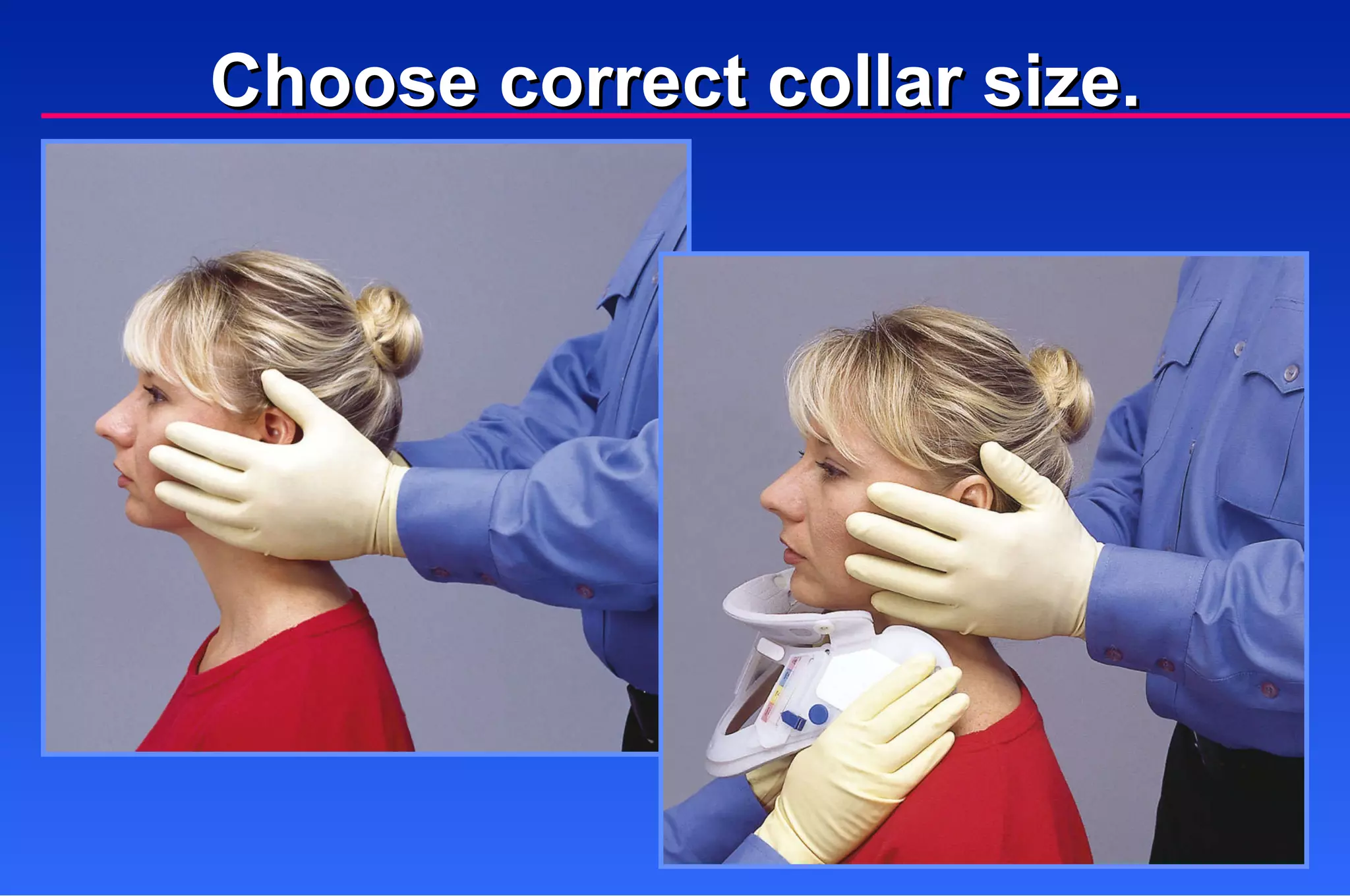
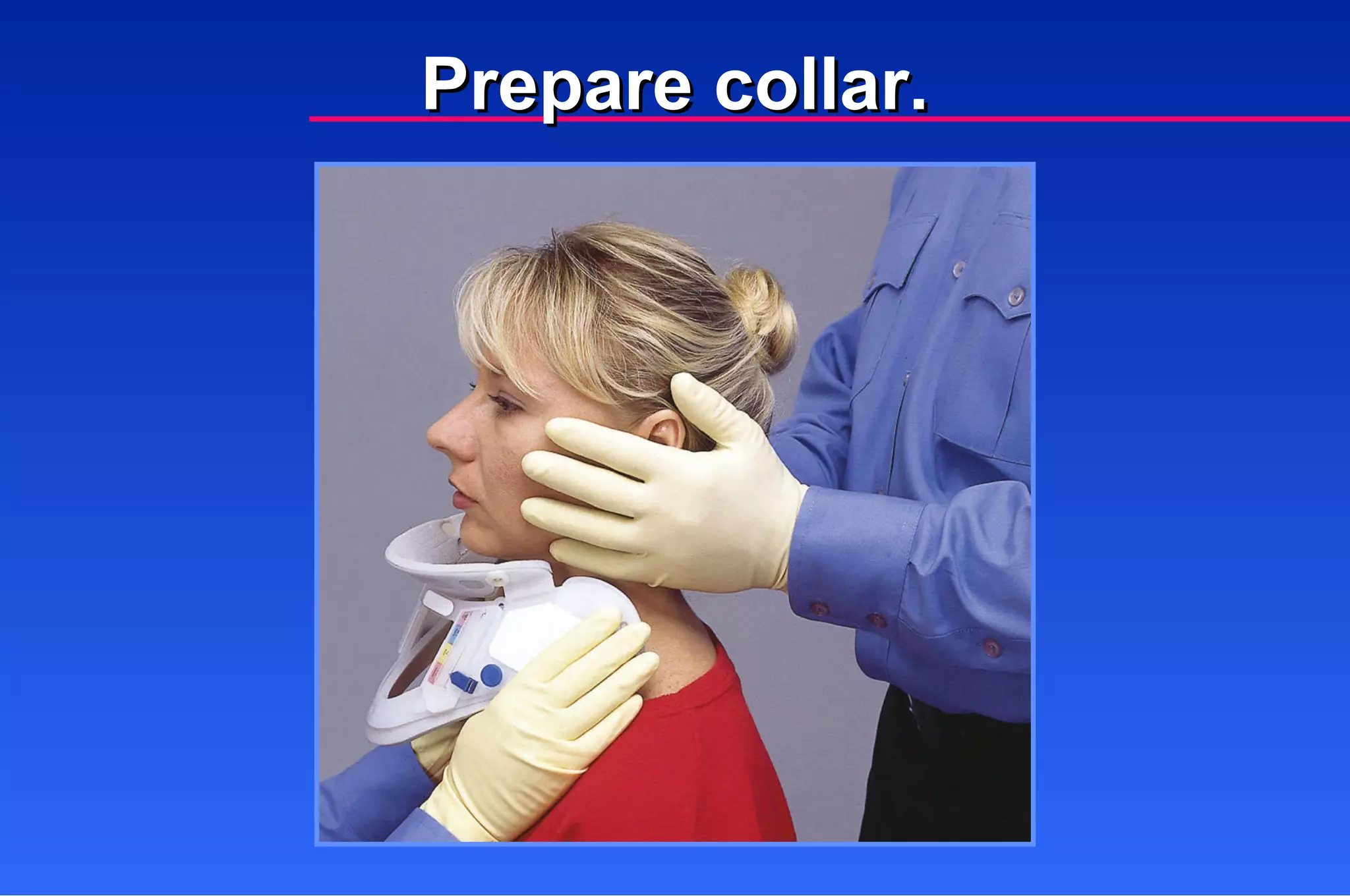
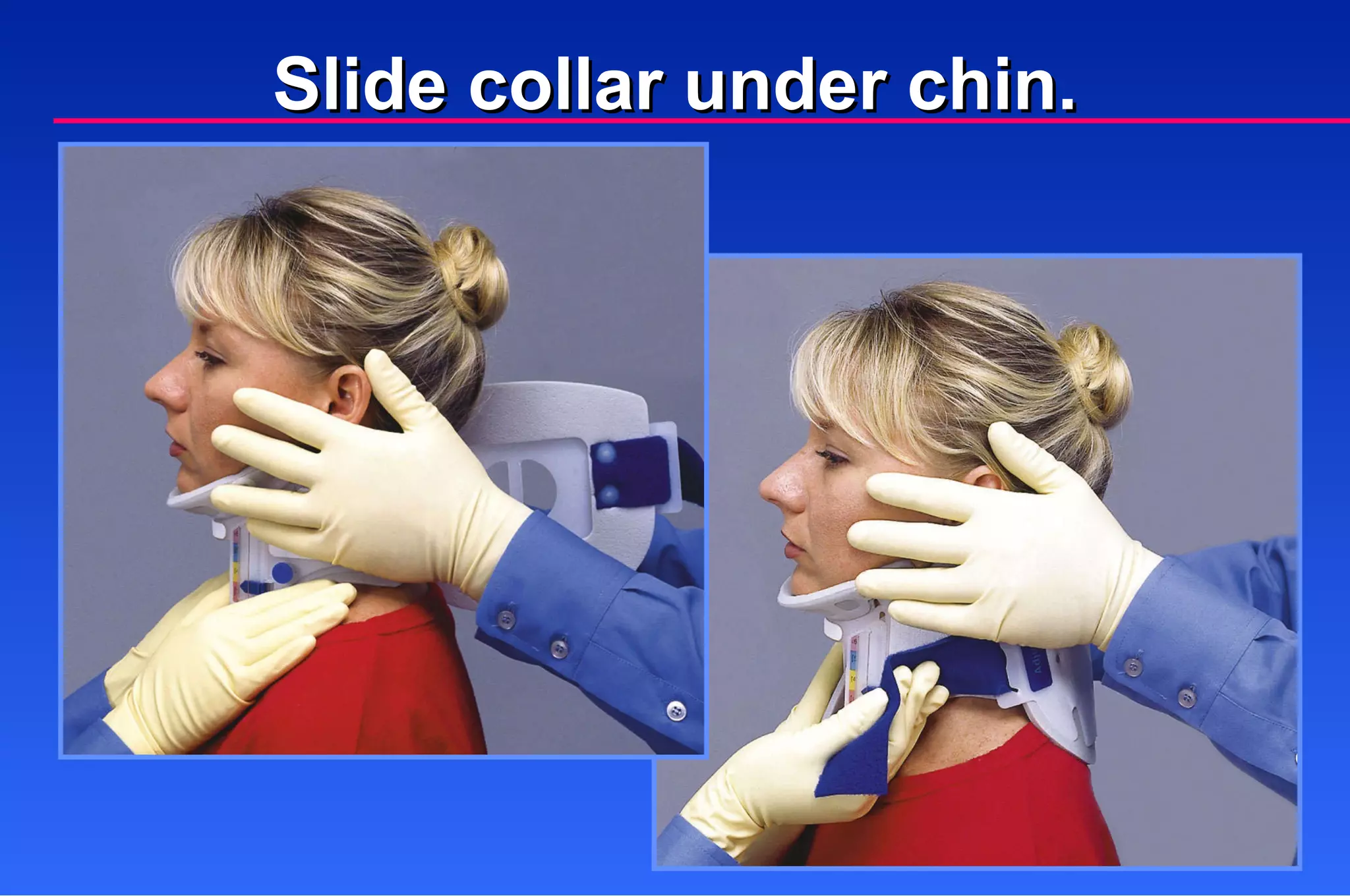
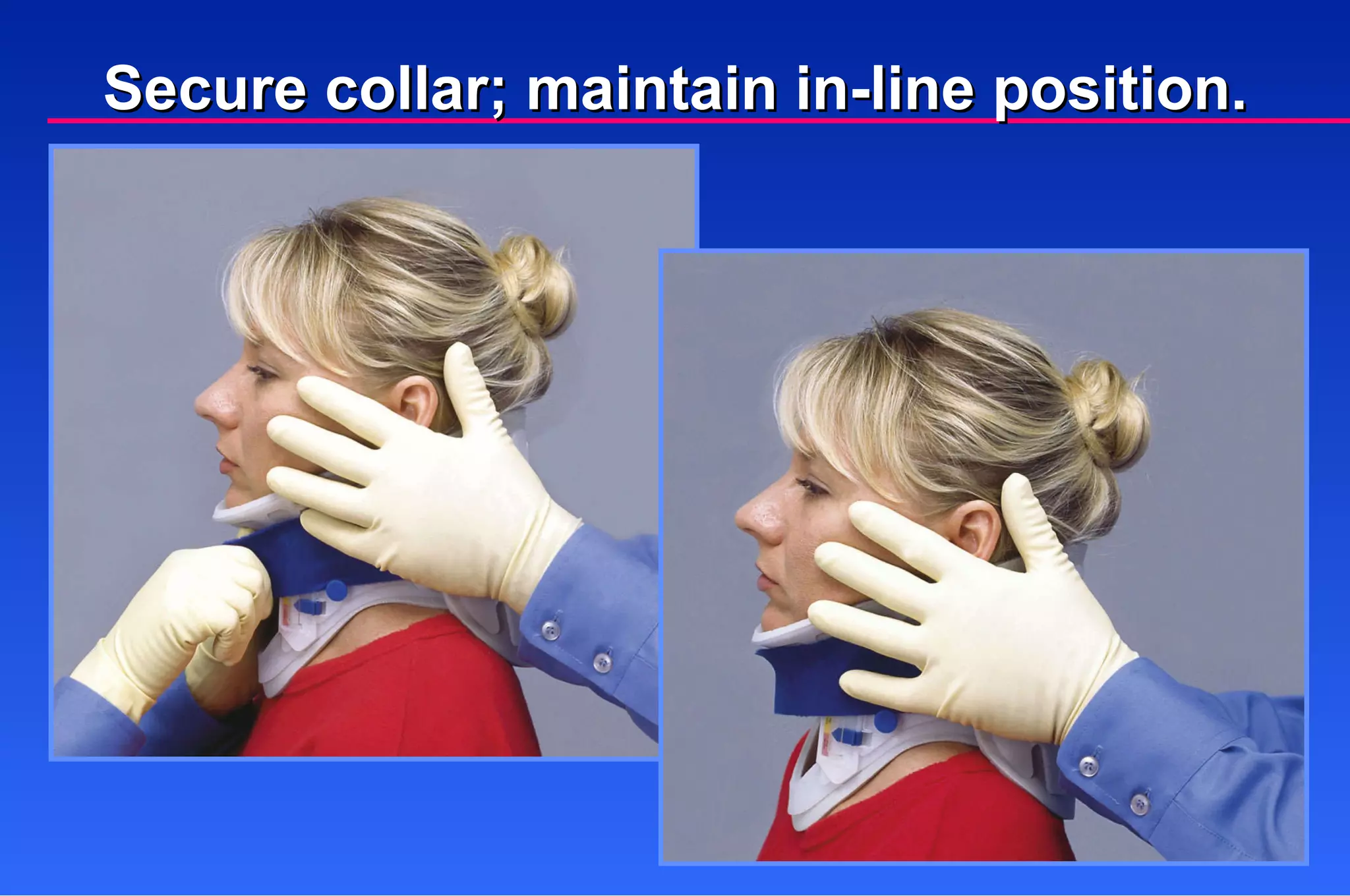
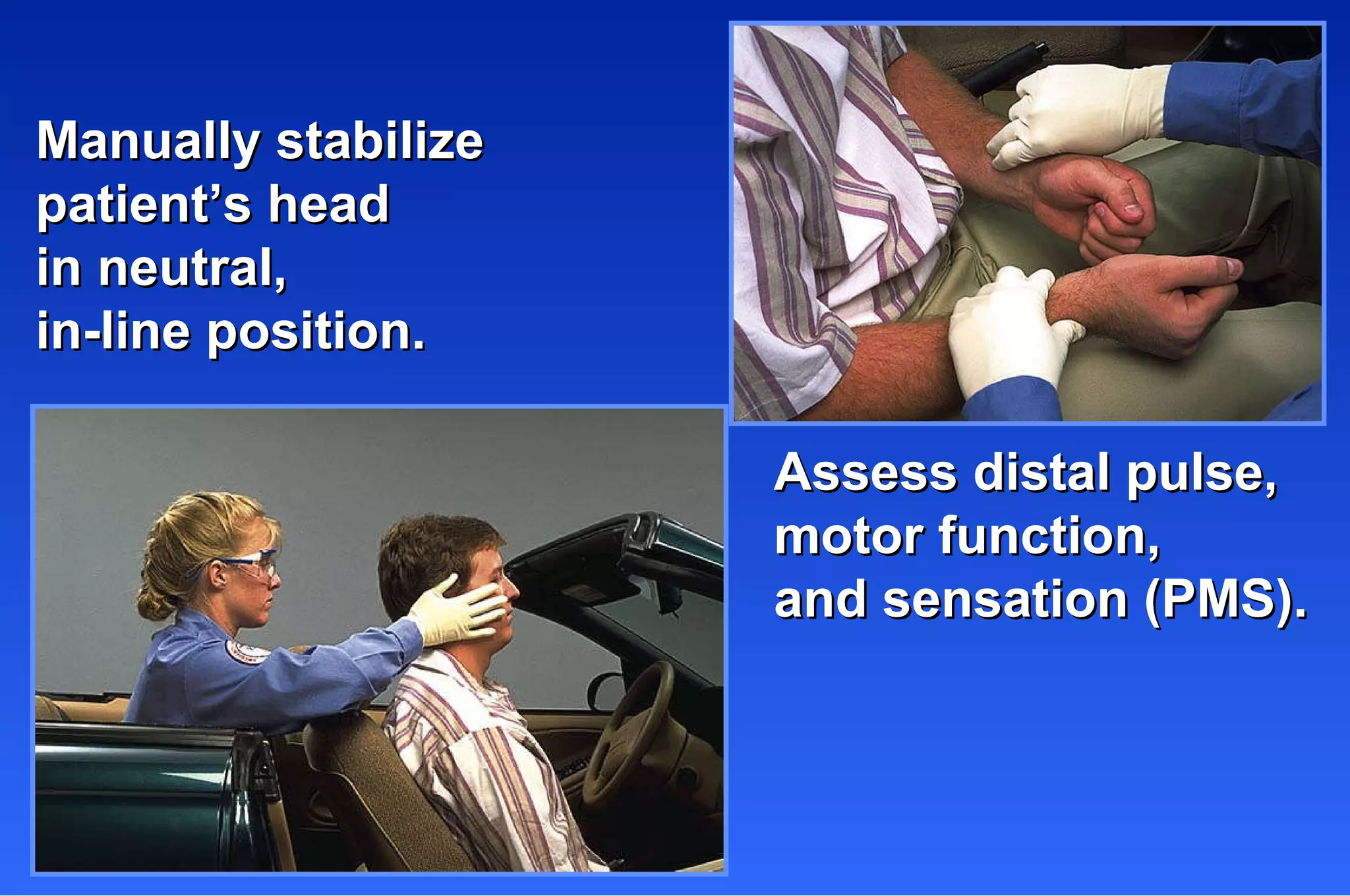
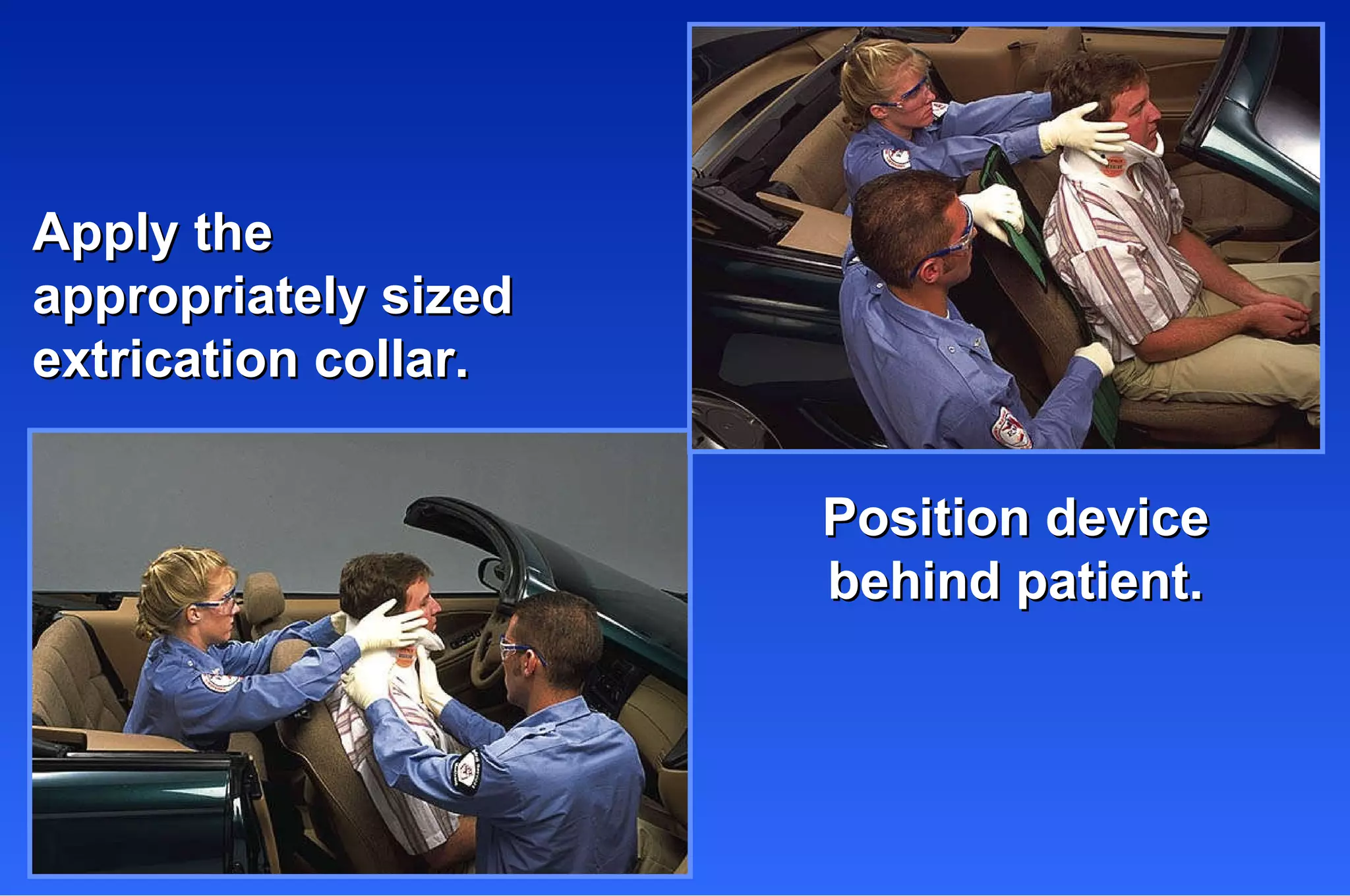
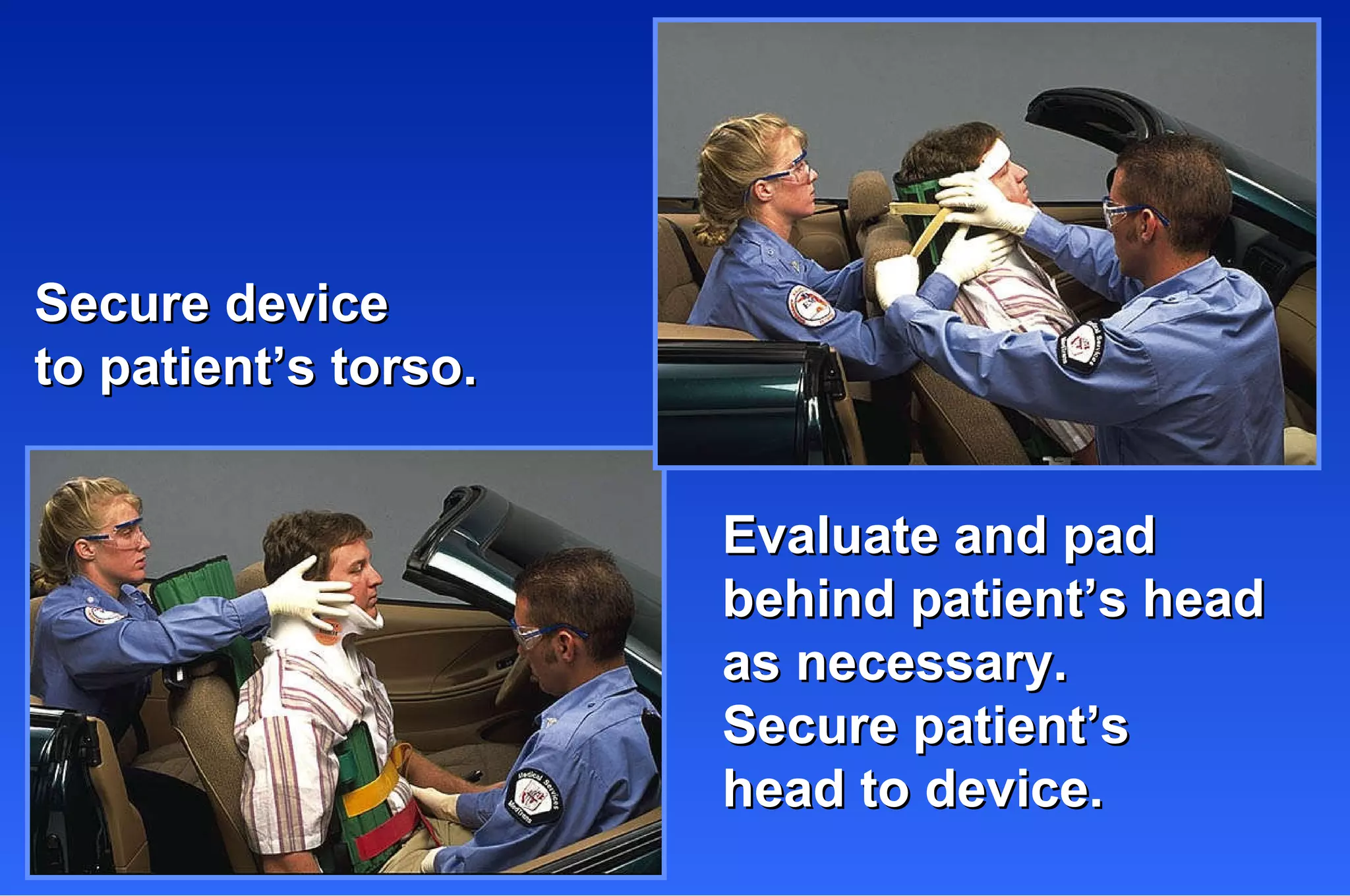
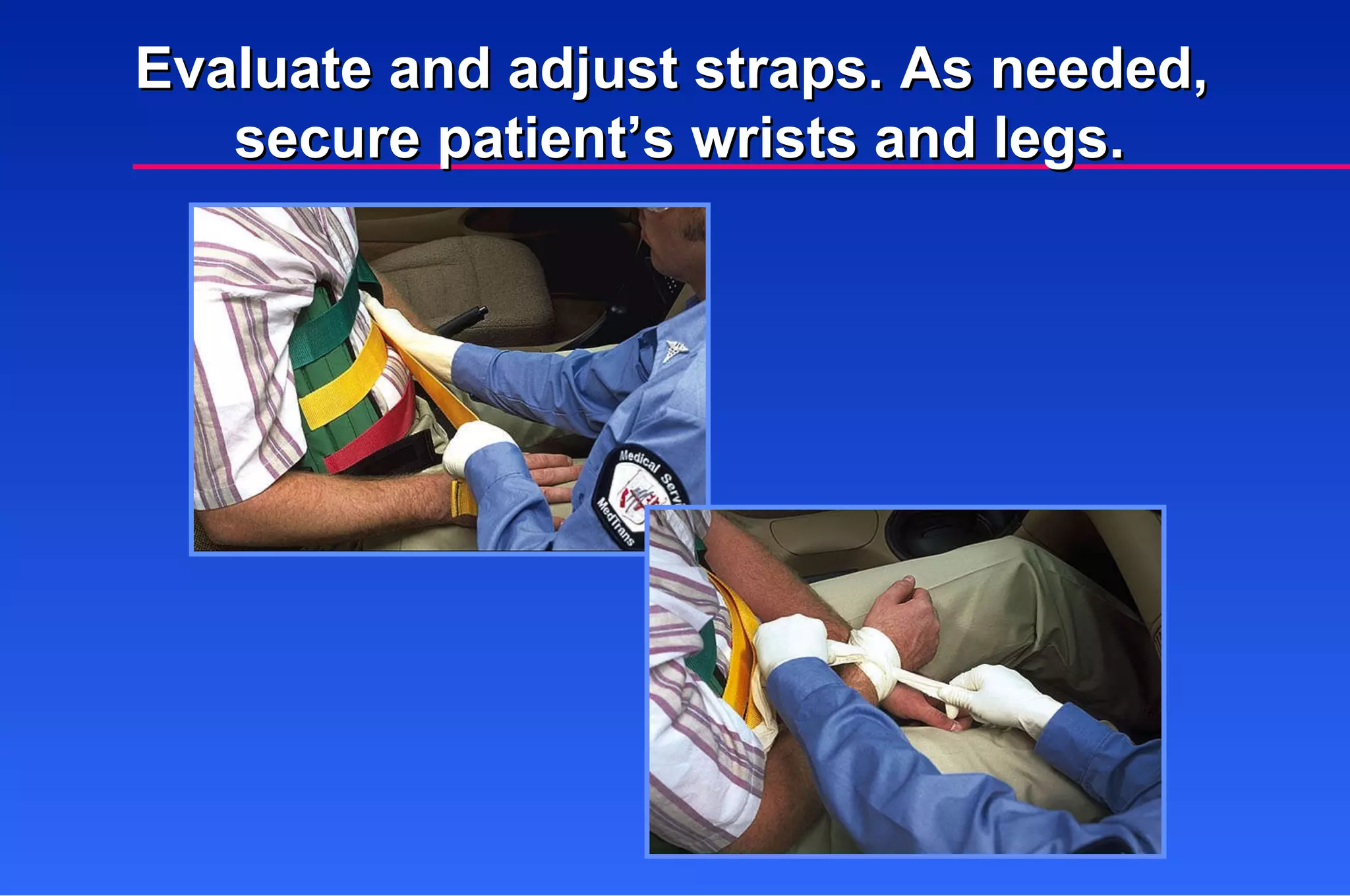
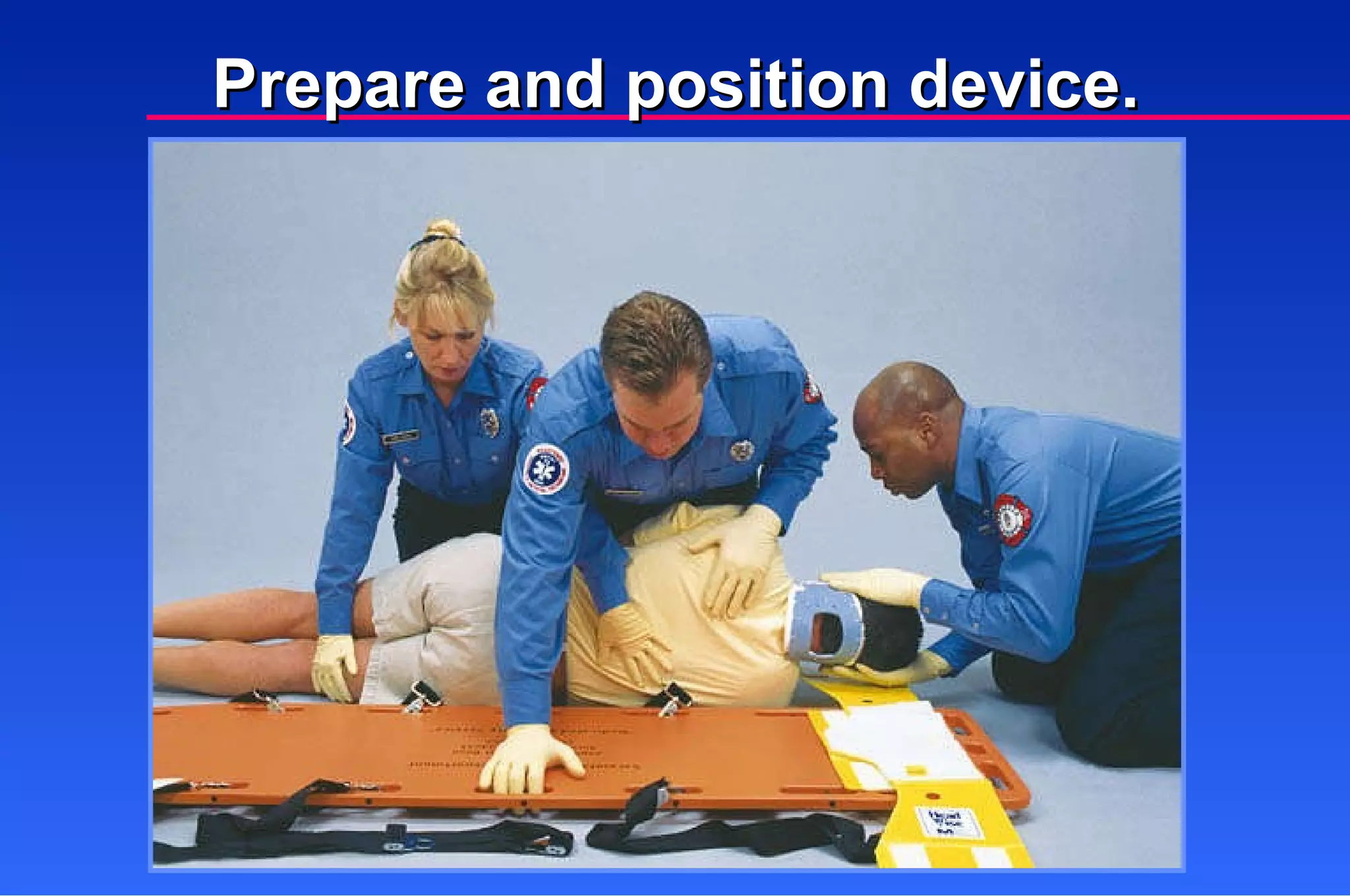
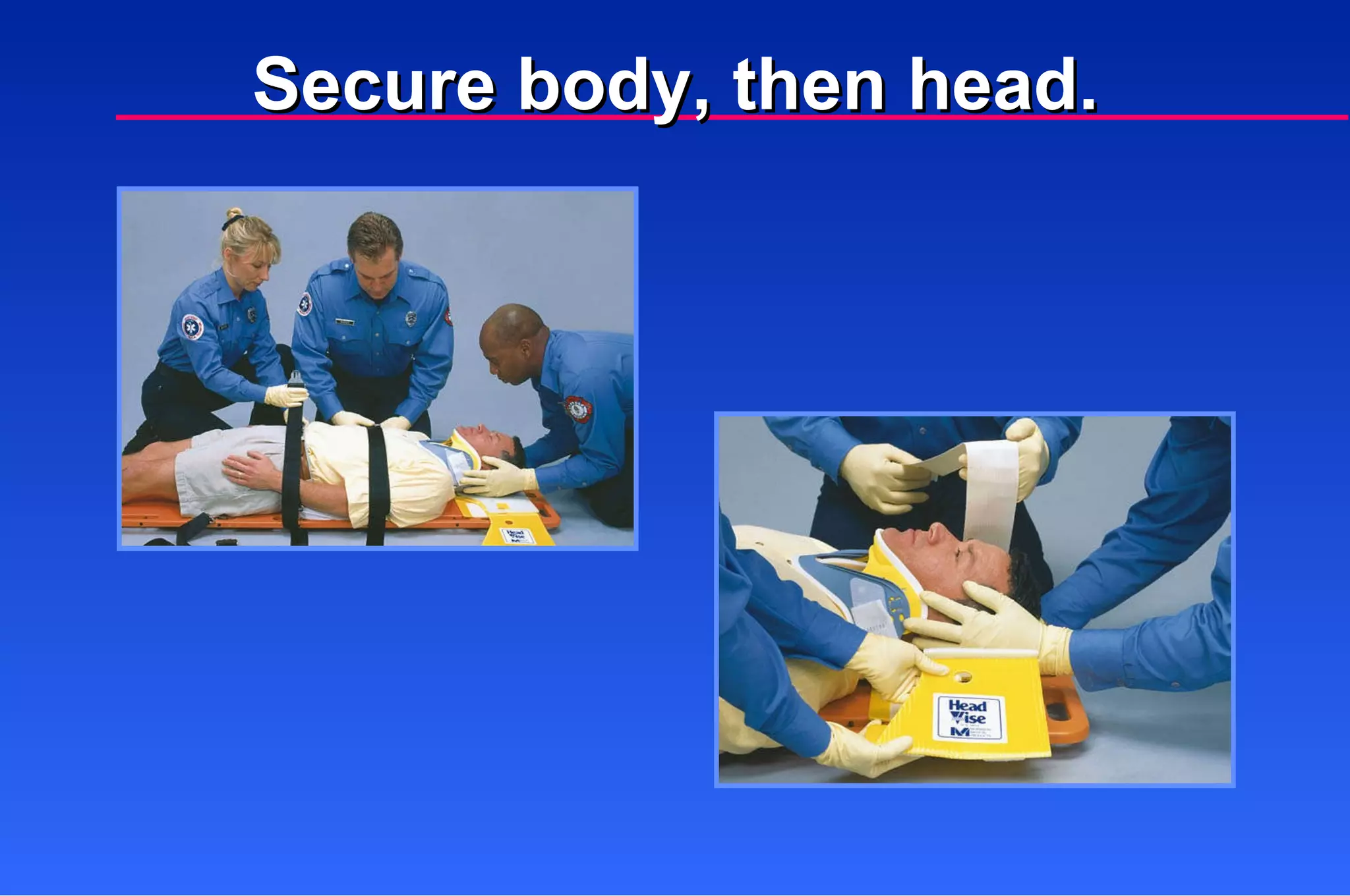
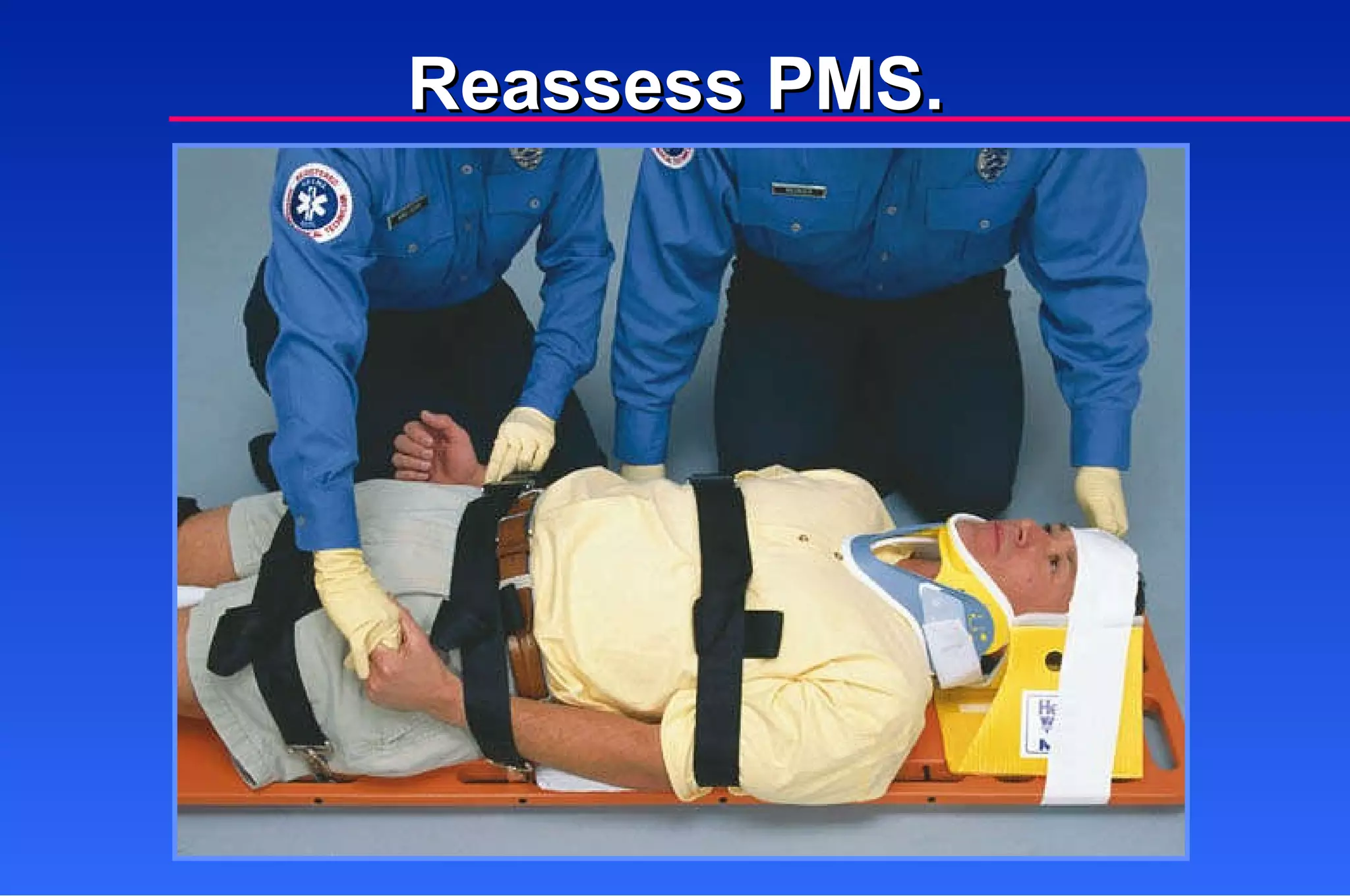
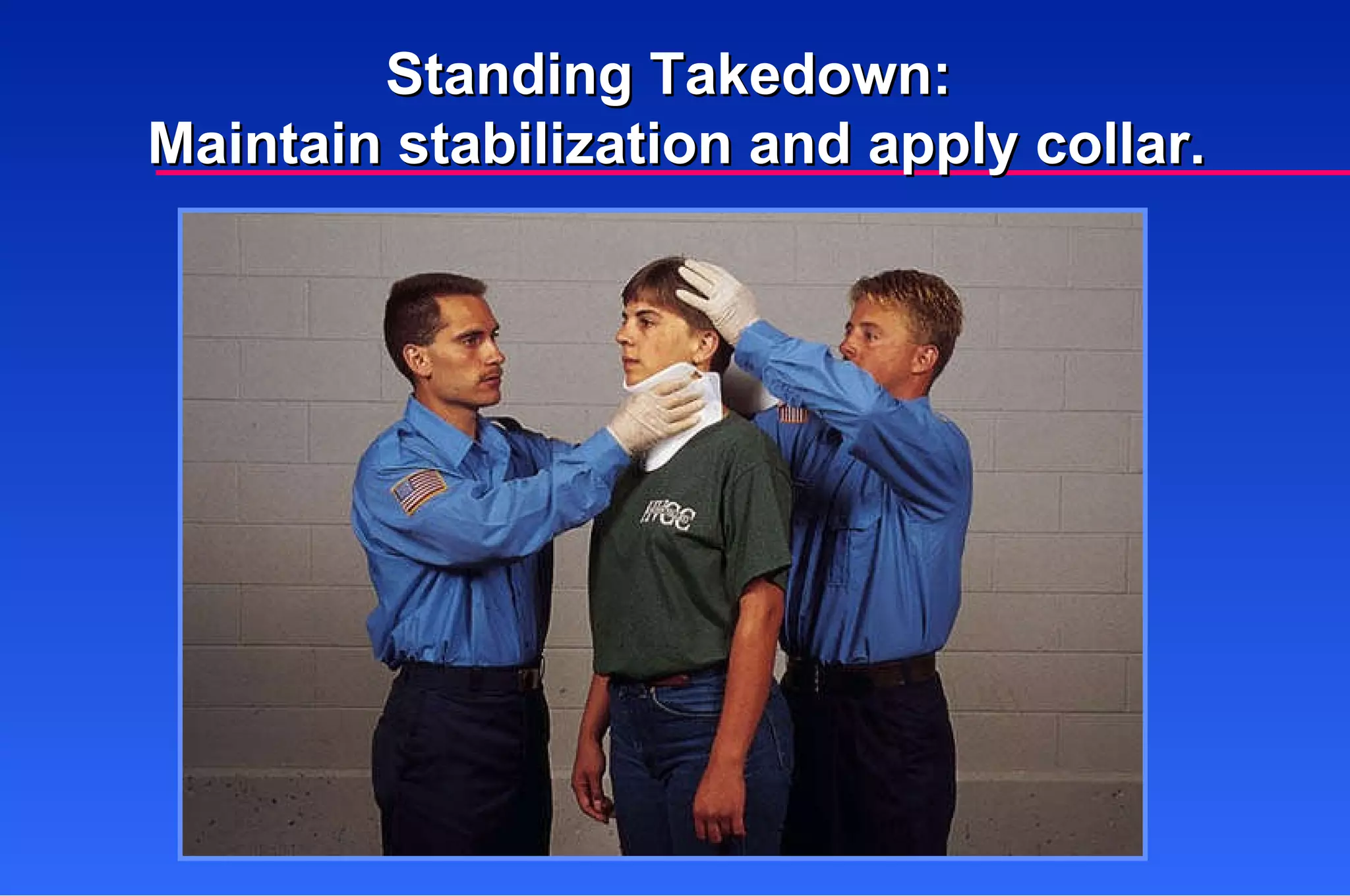
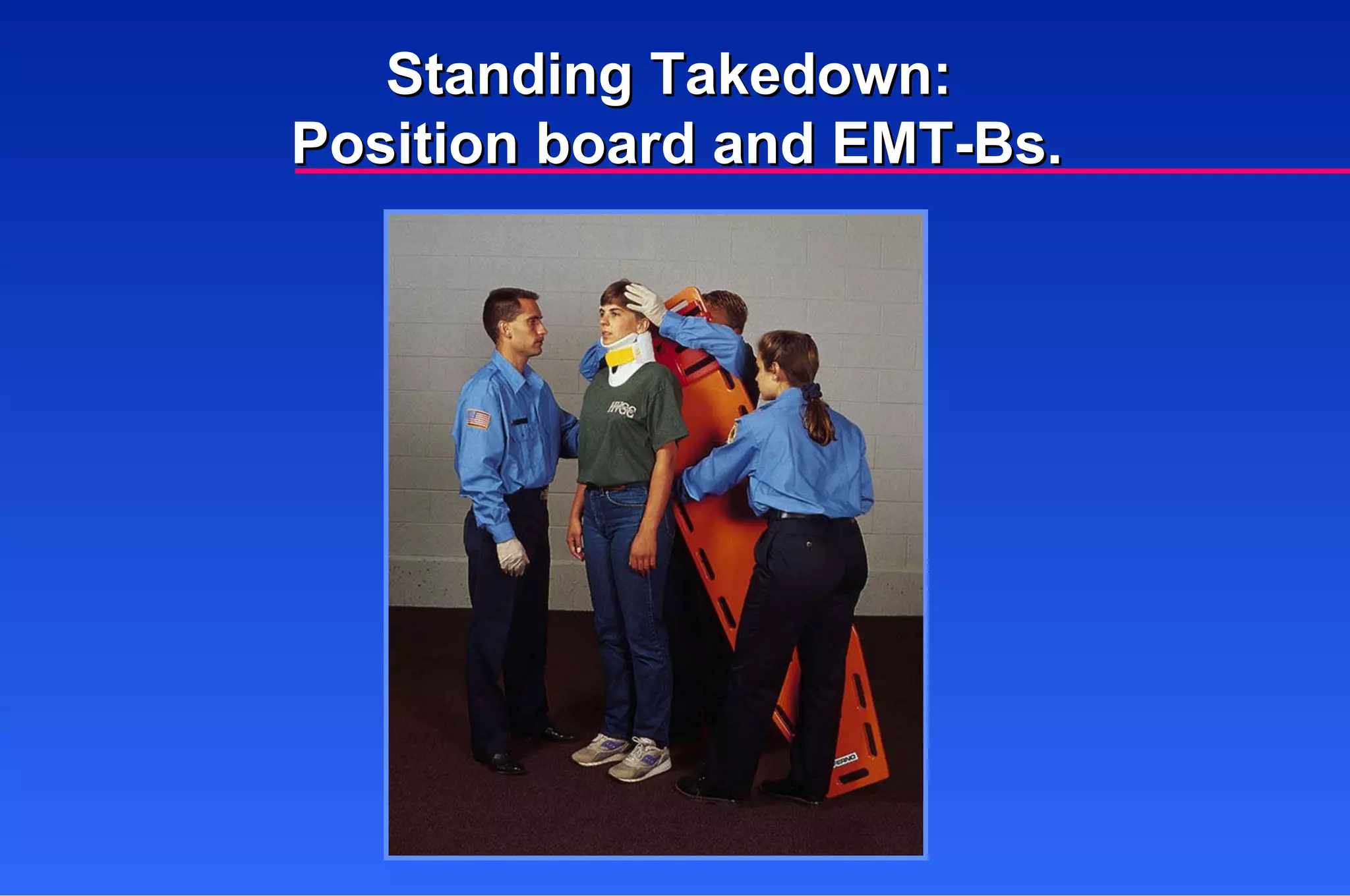
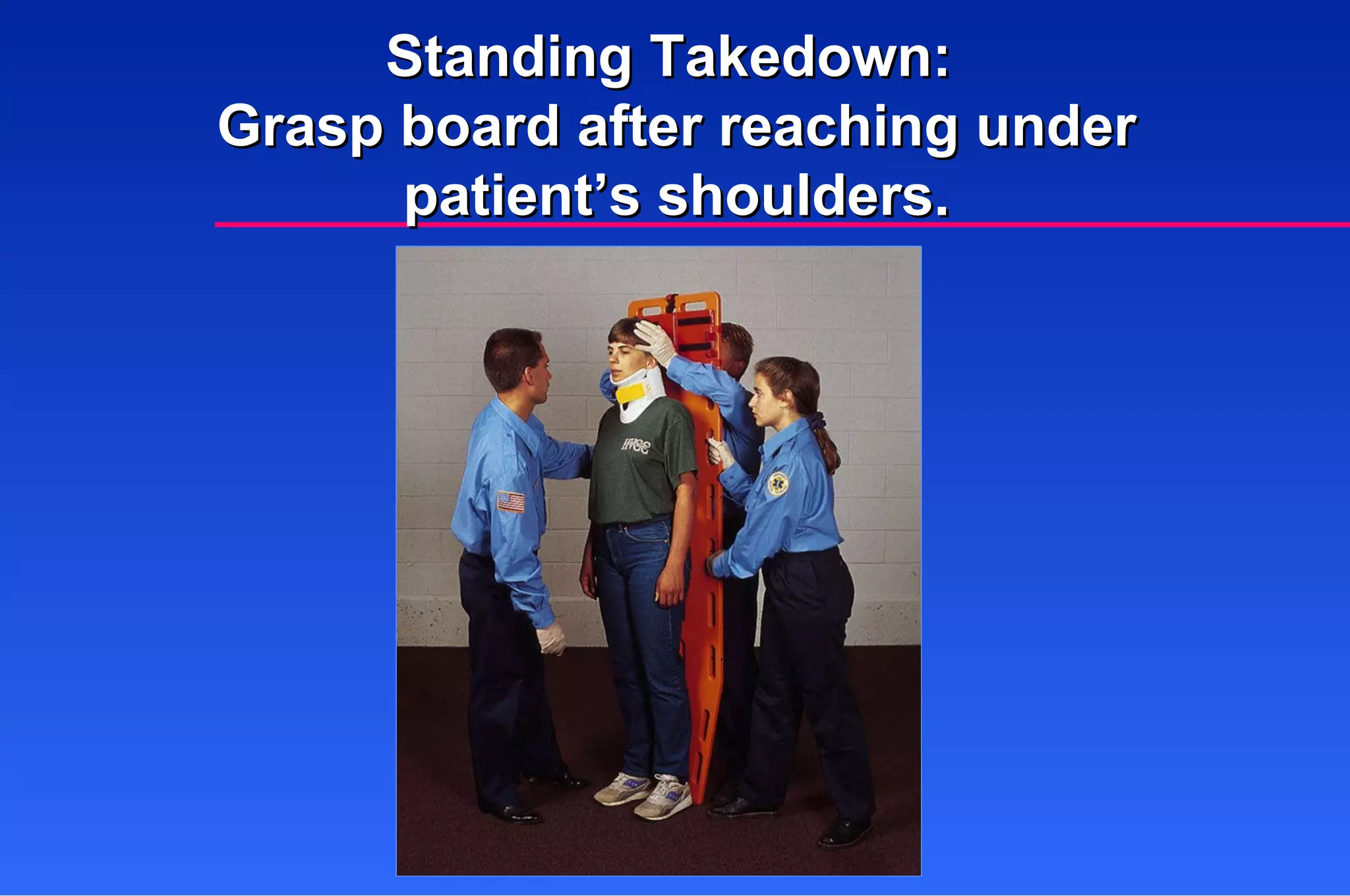
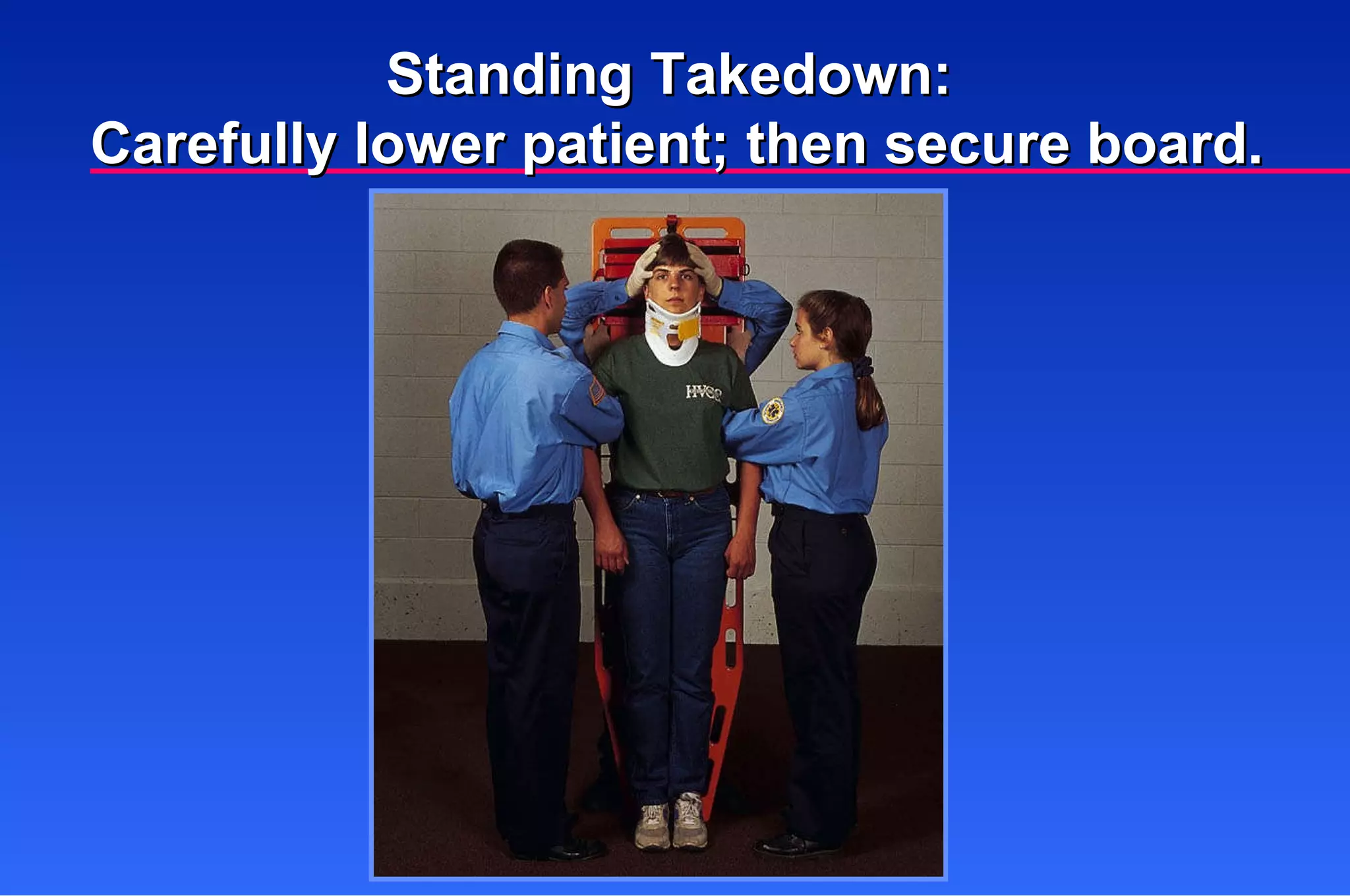
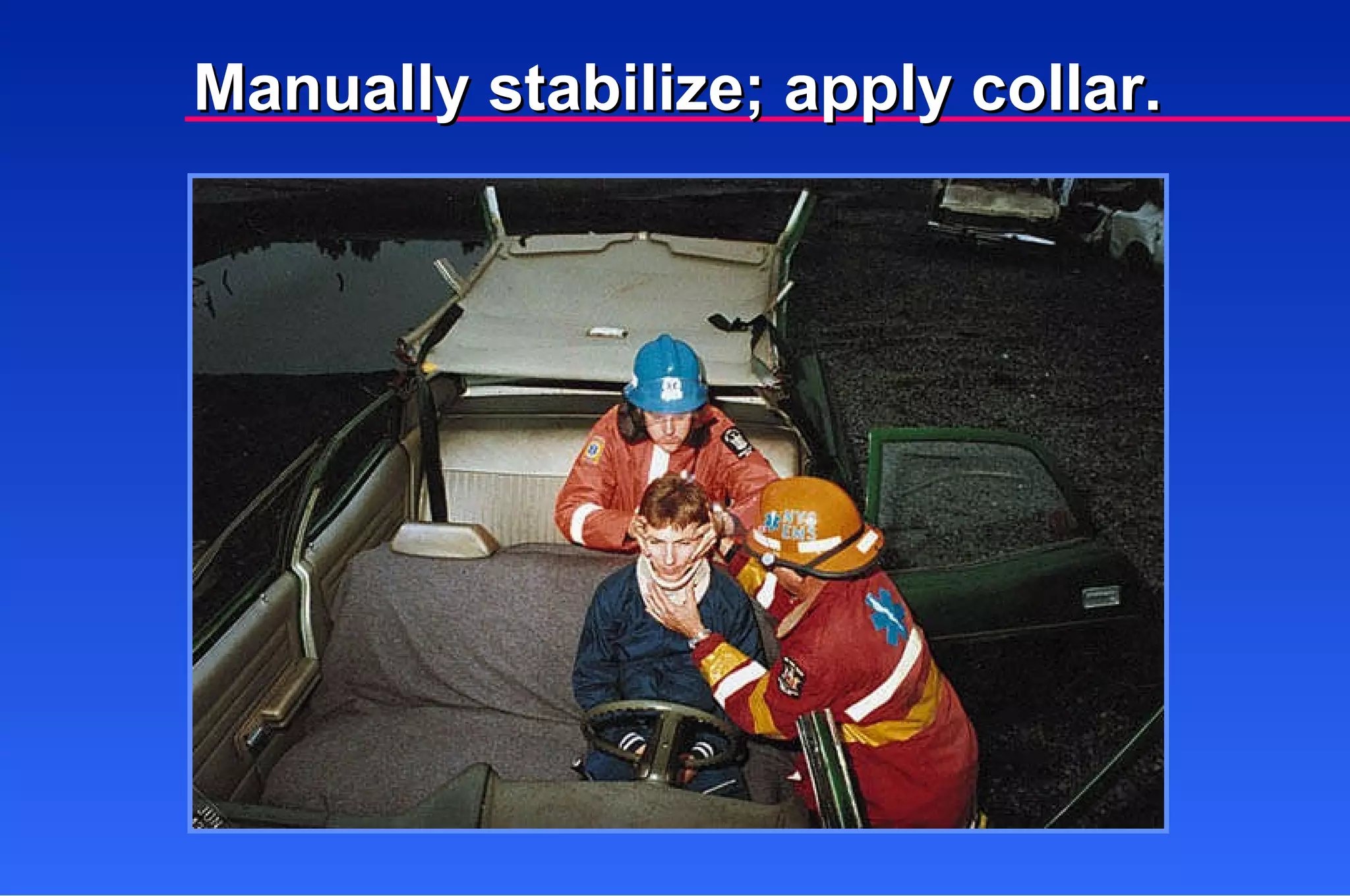
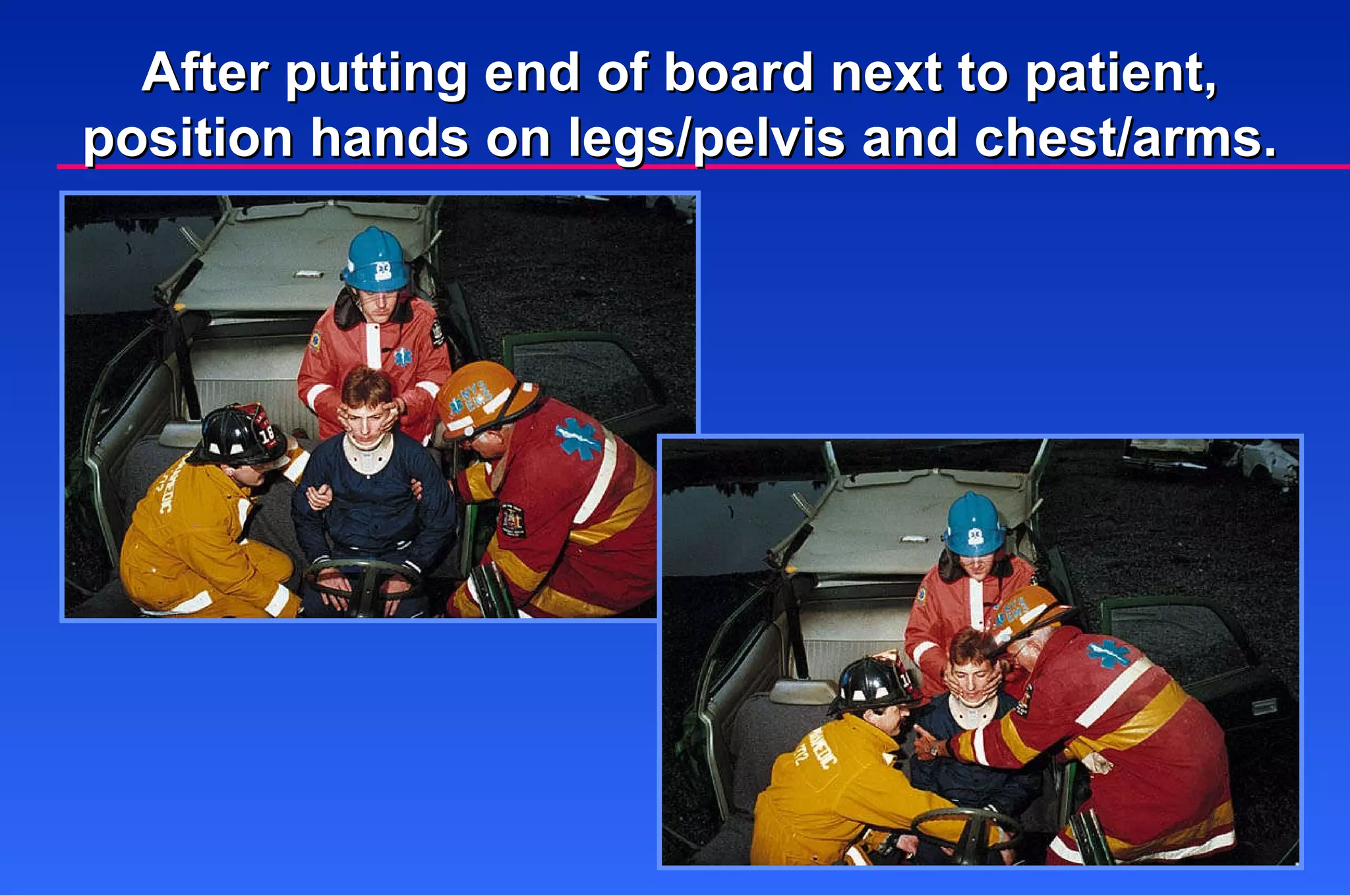
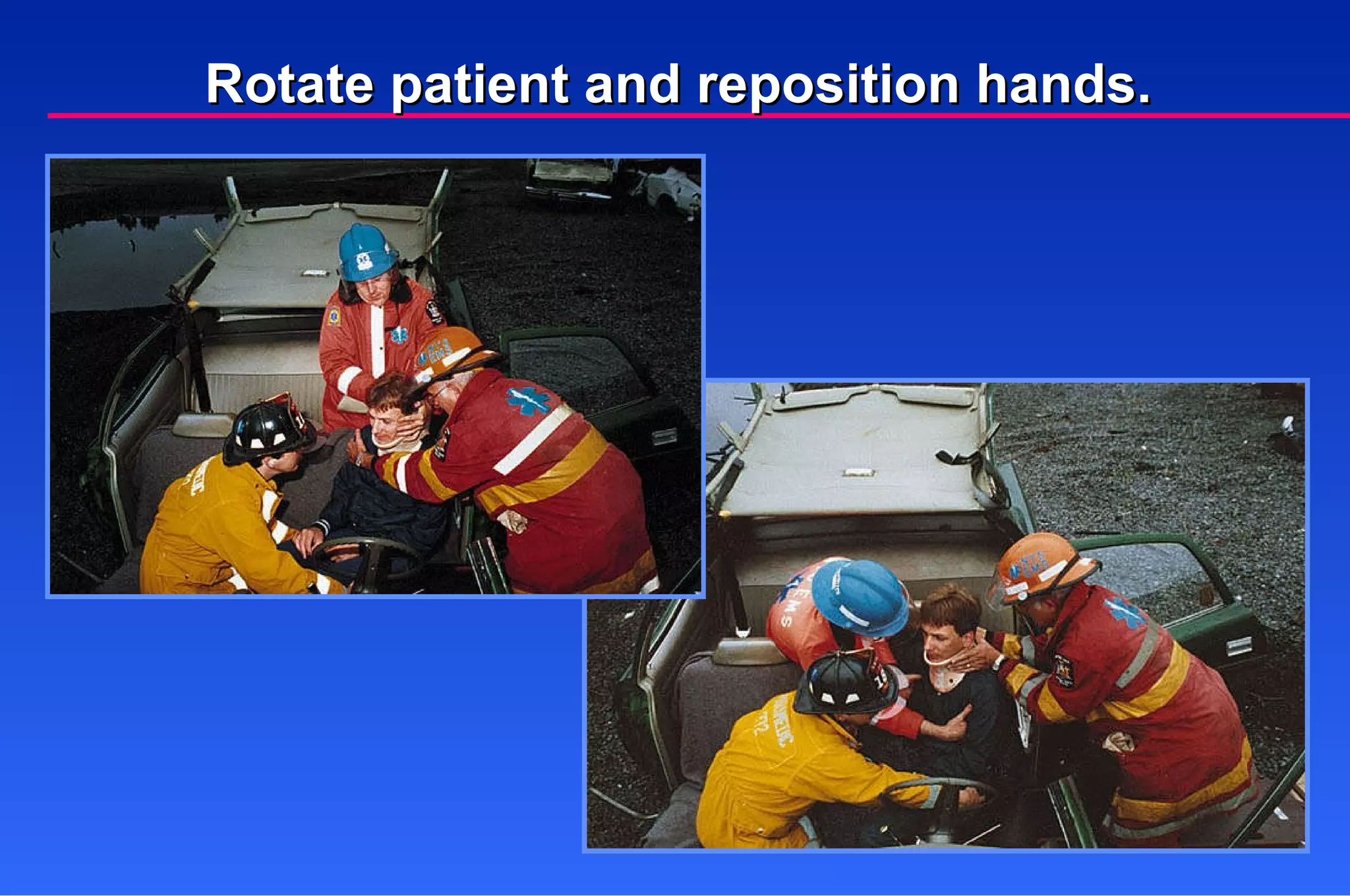
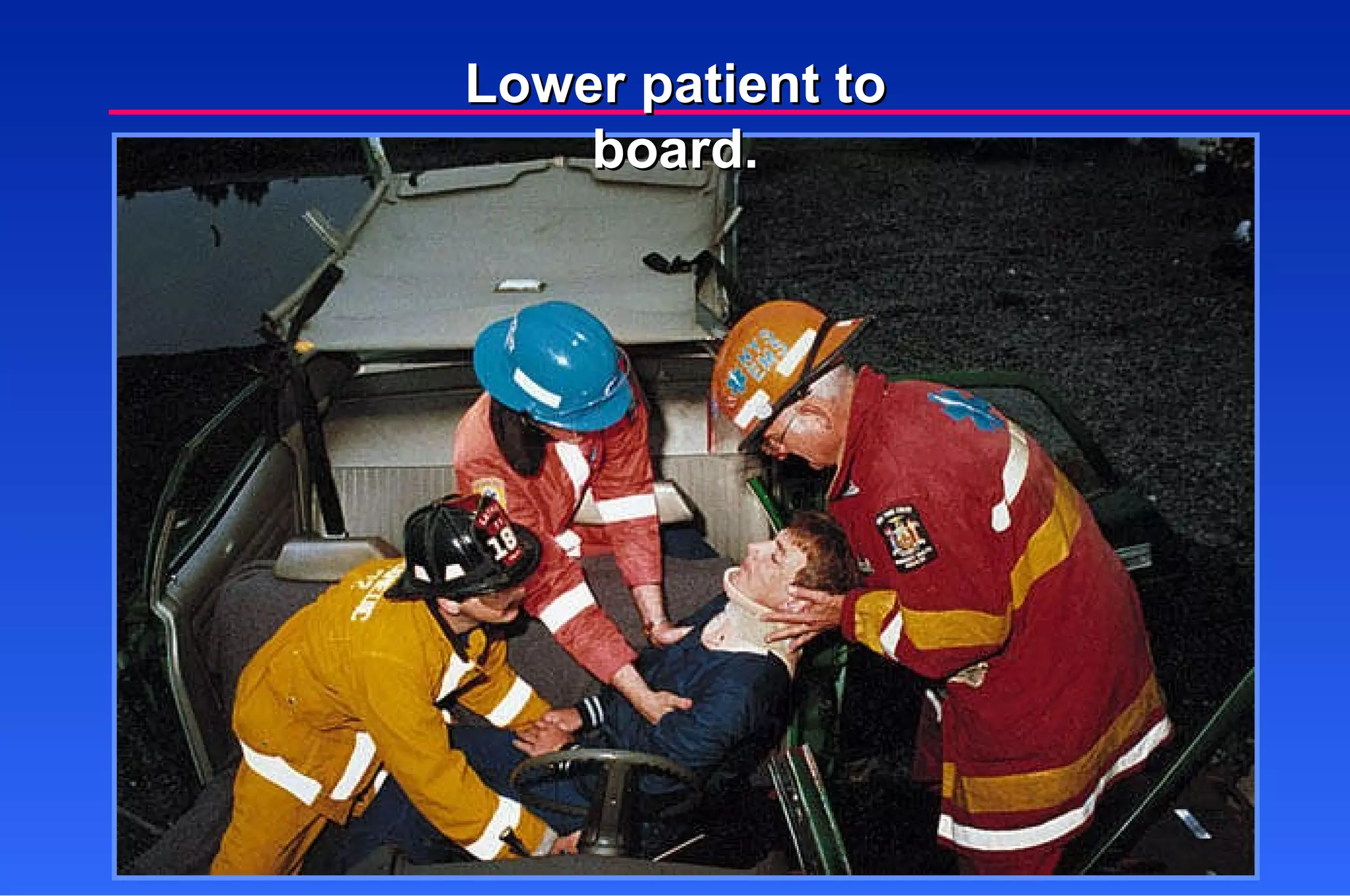
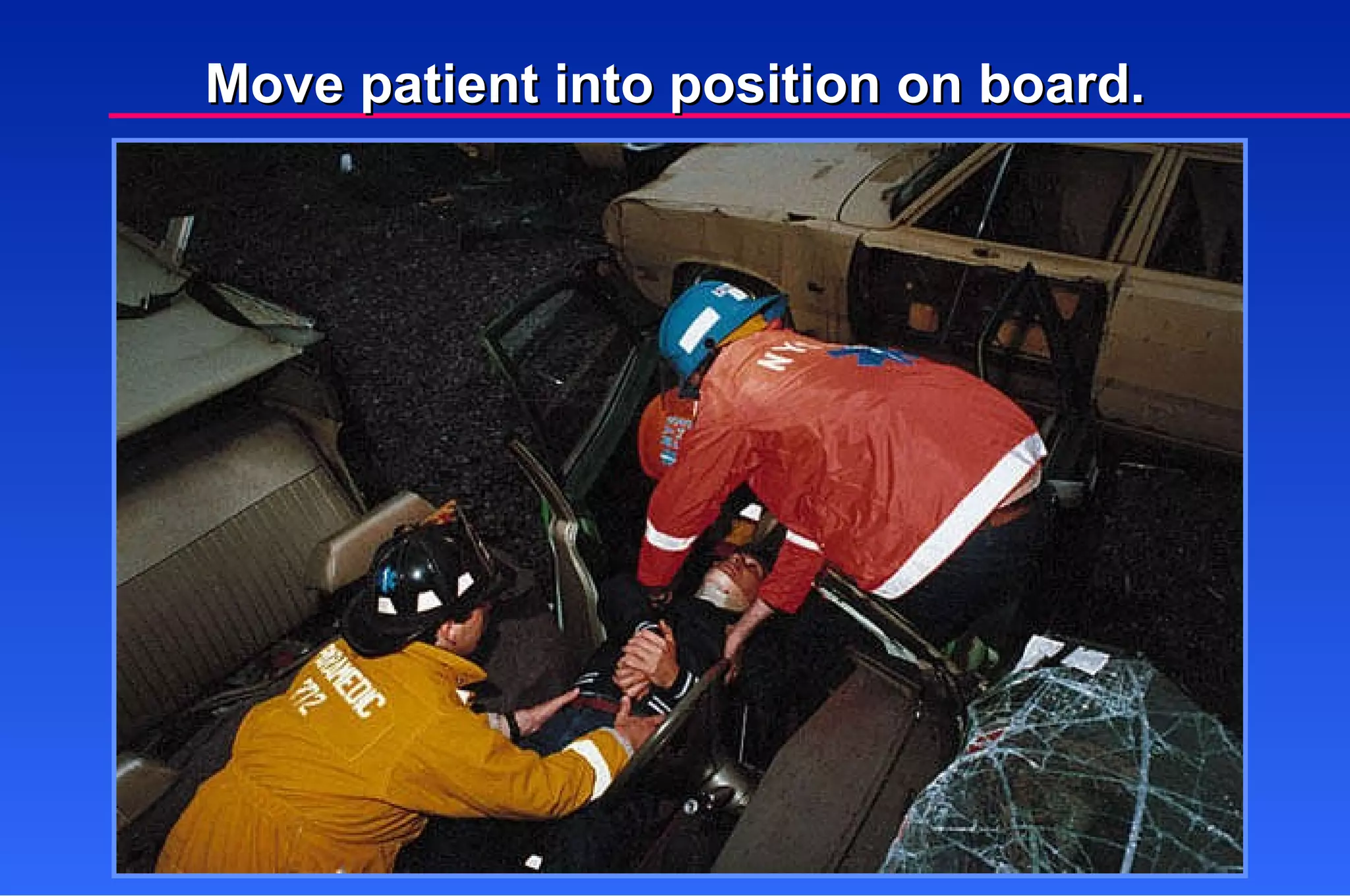
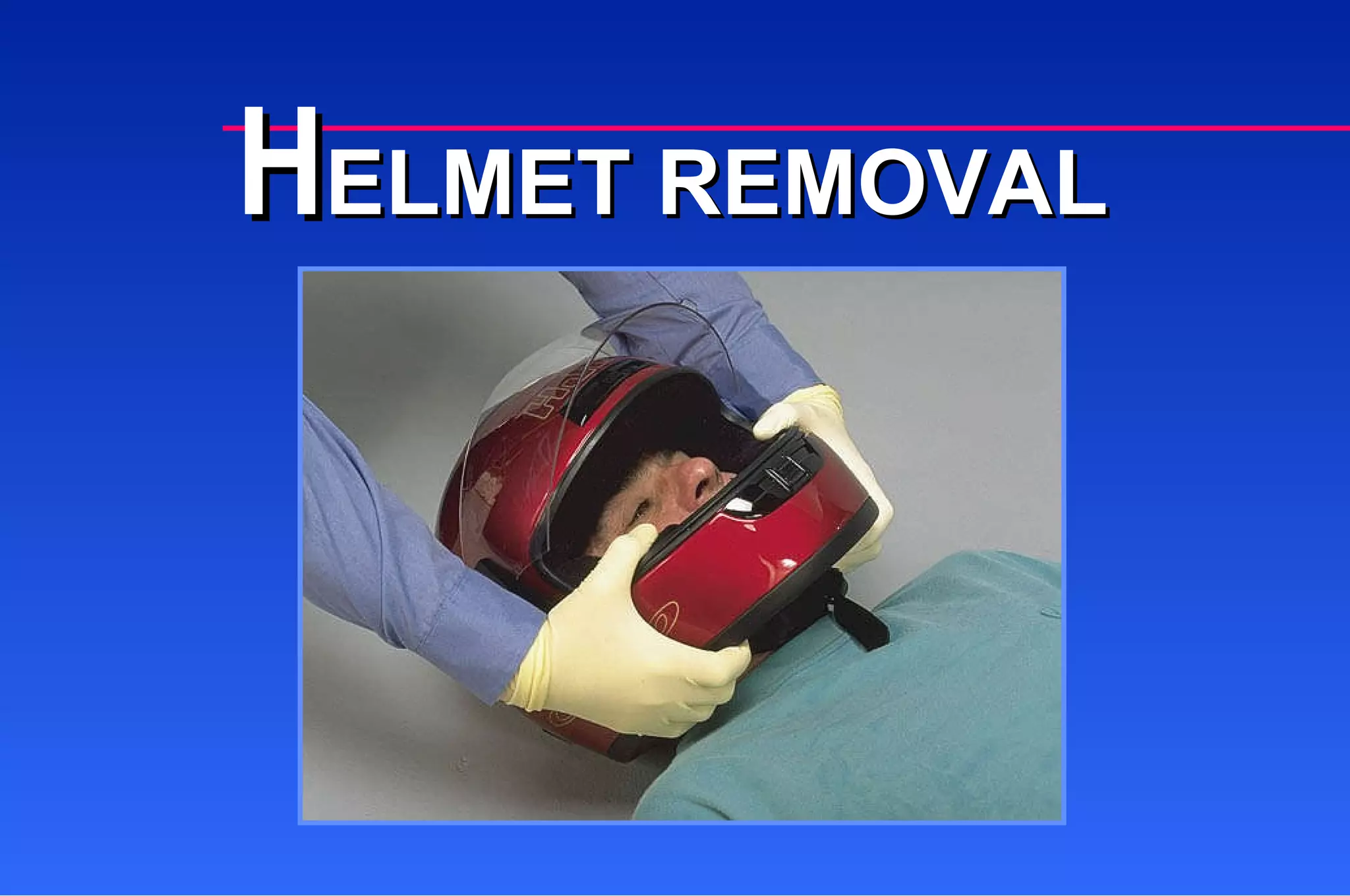
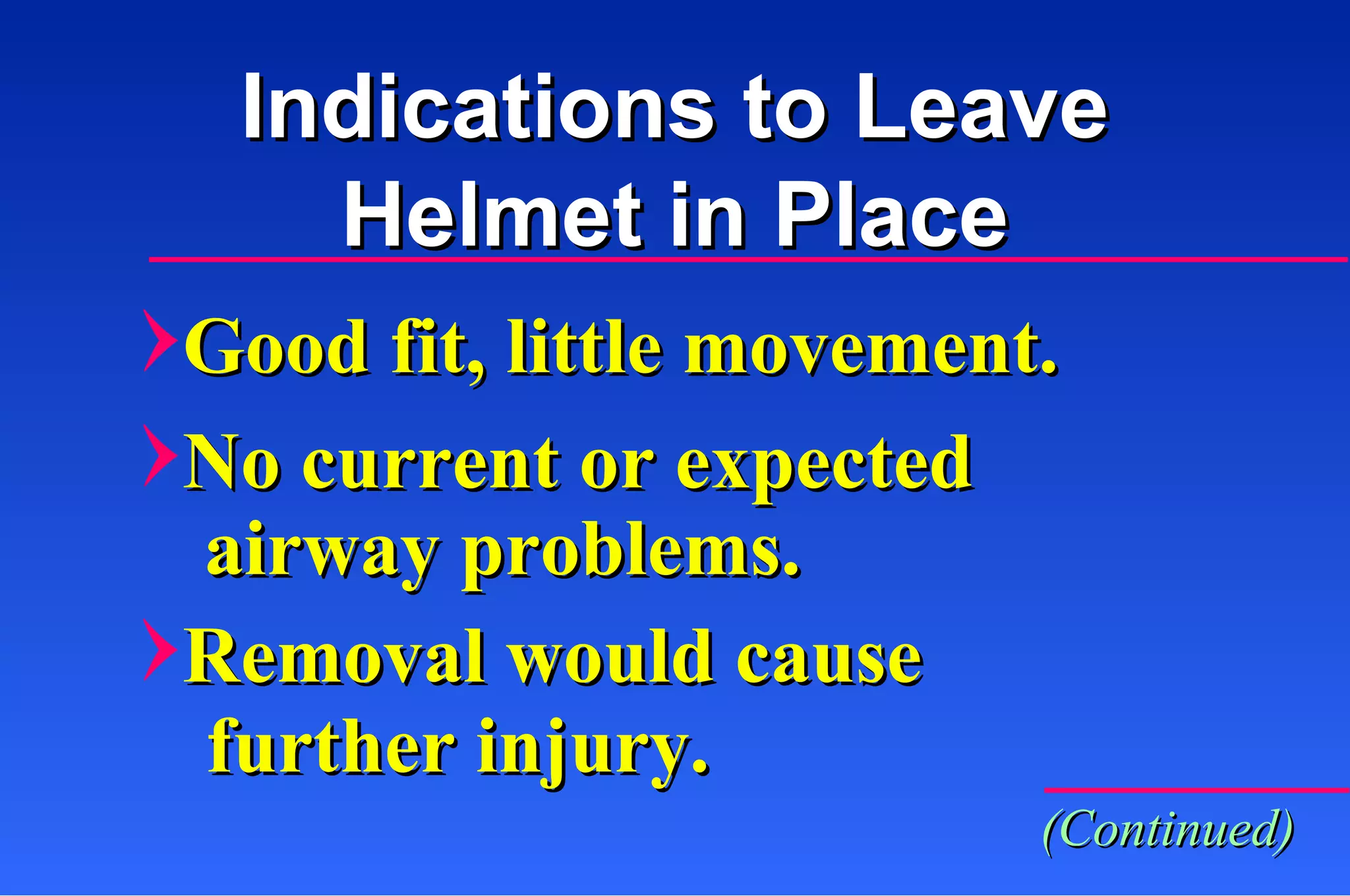
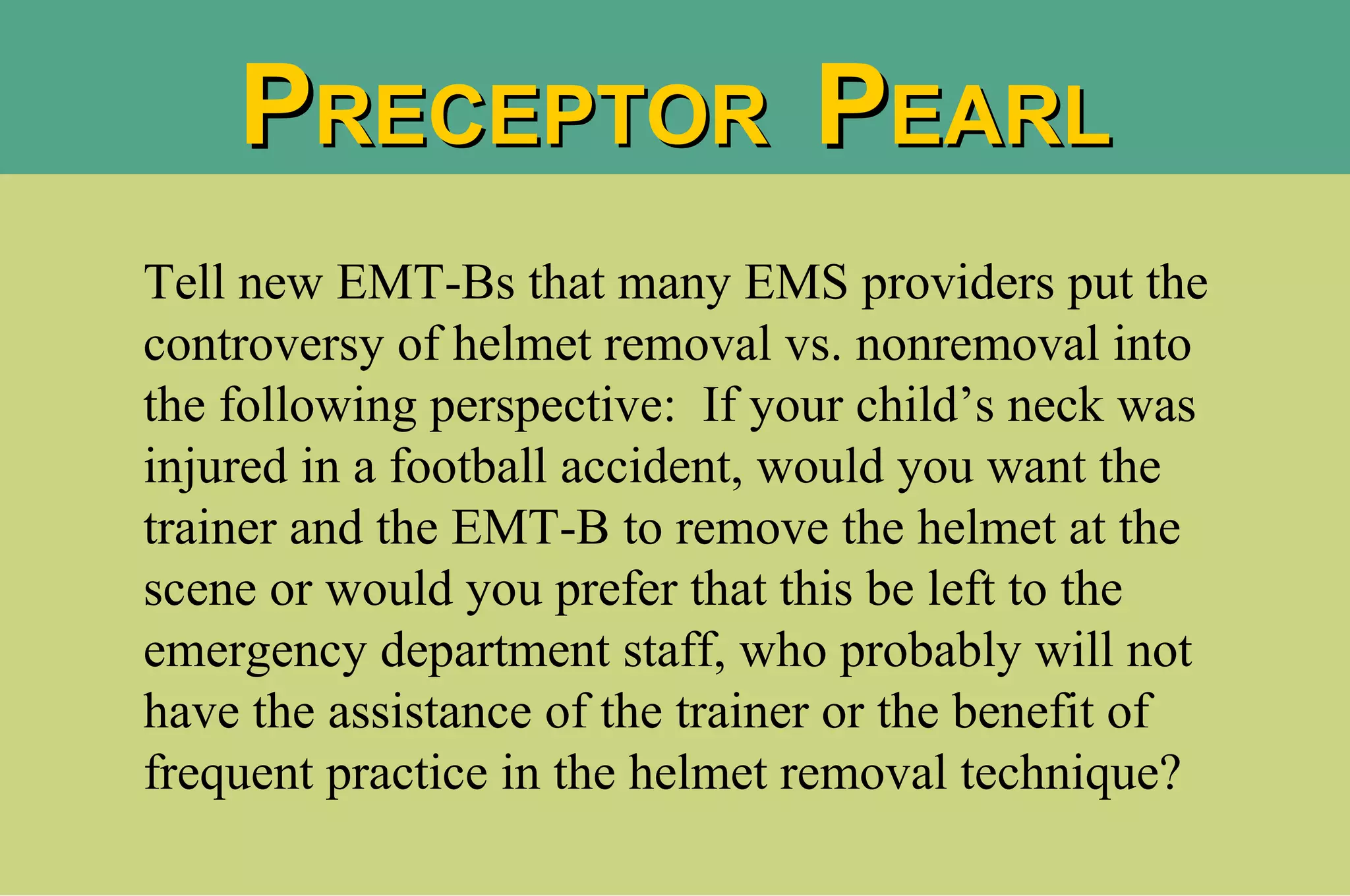
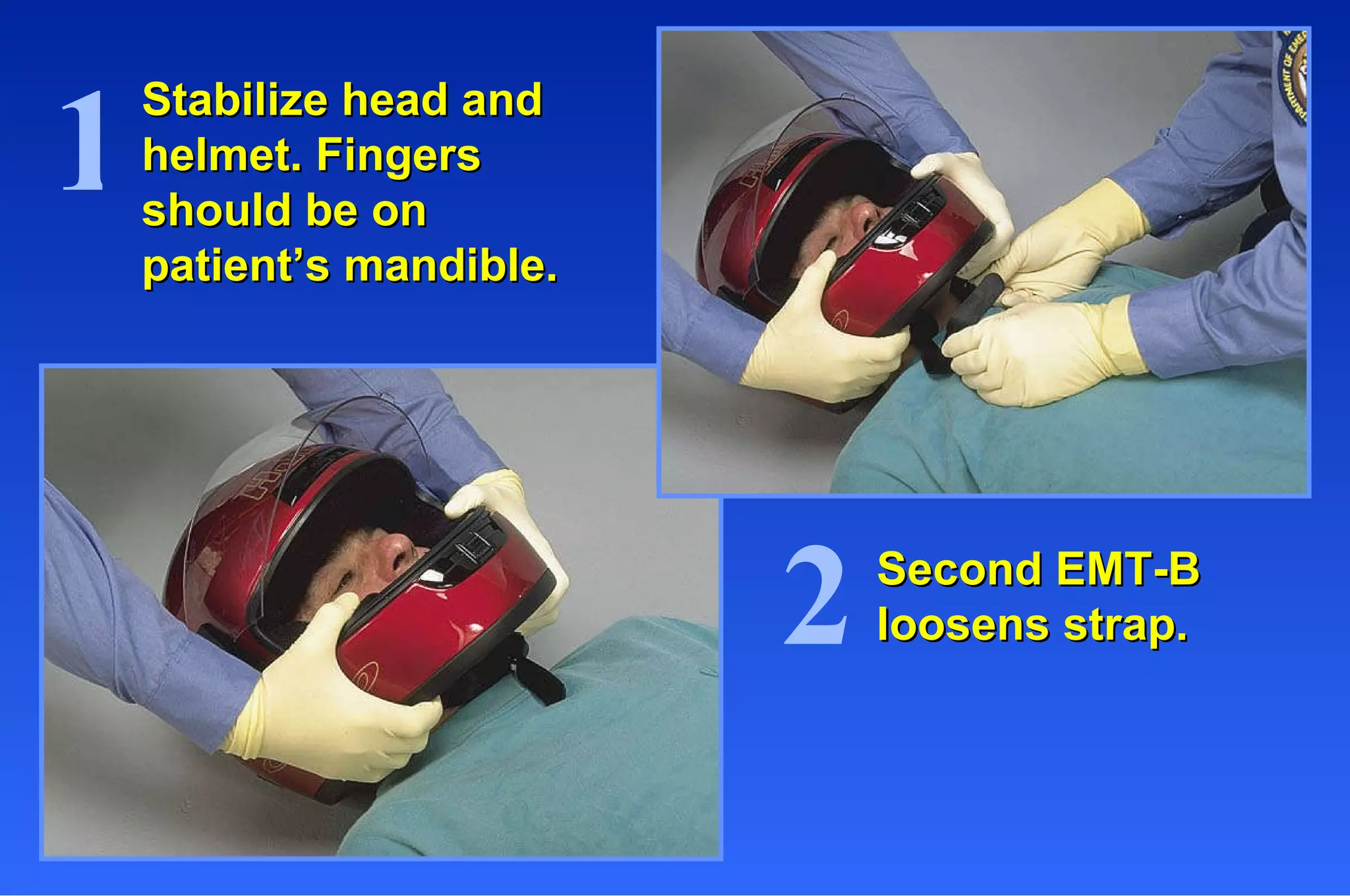
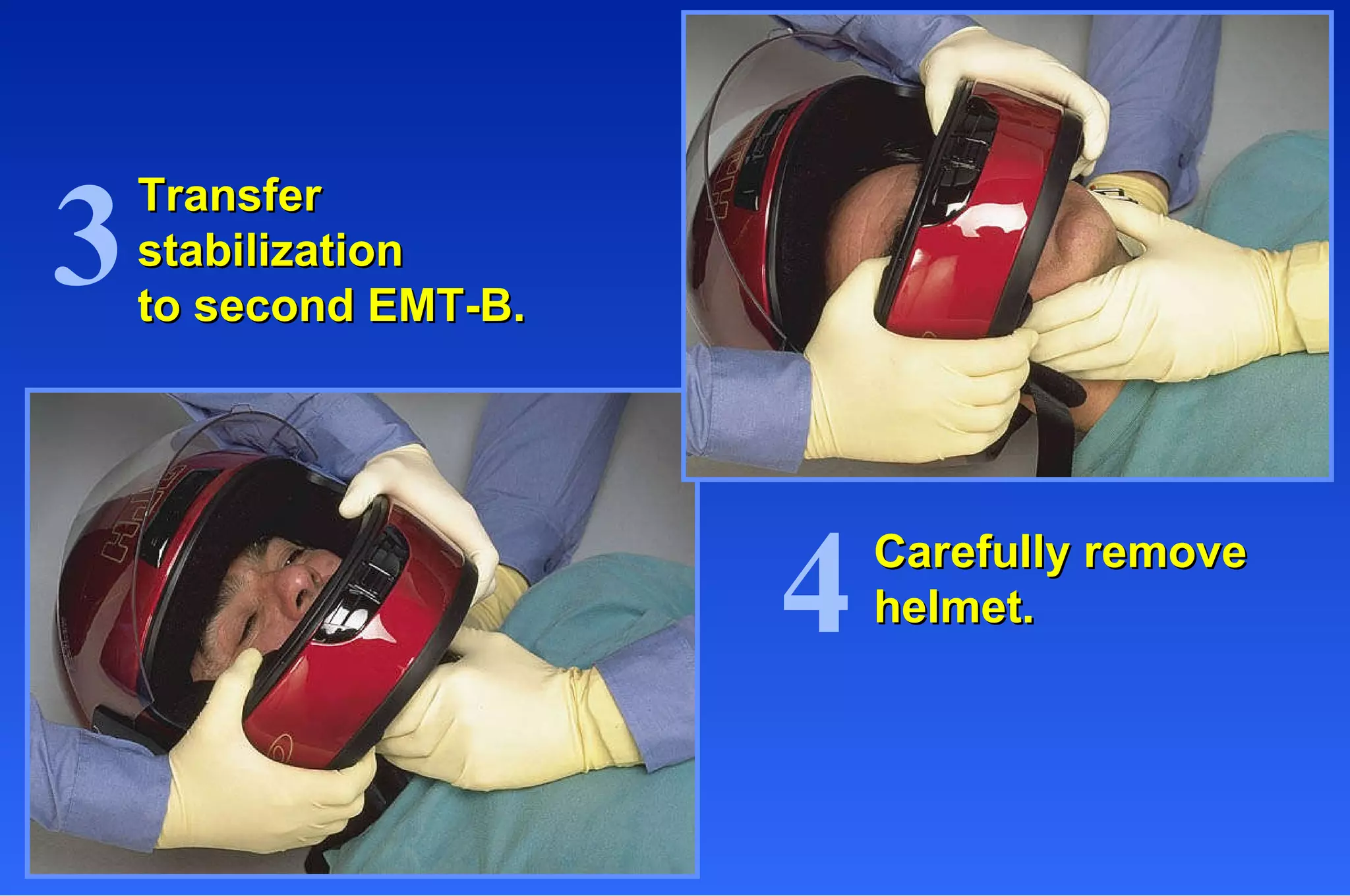
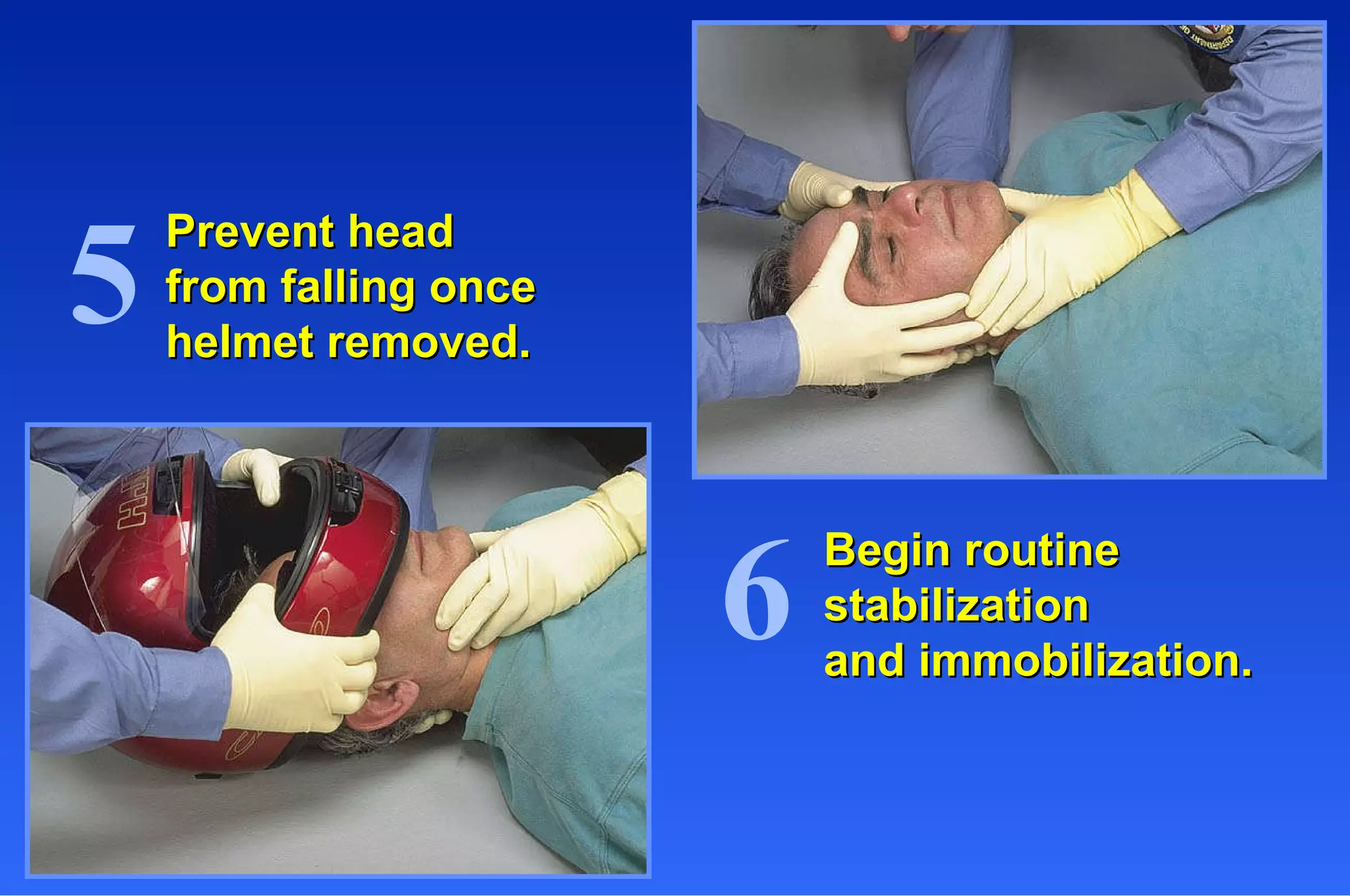
This document provides information on injuries to the head and spine, including mechanisms of injury, patient assessment signs and symptoms, and emergency care procedures. It discusses direct and indirect brain injuries, types of spinal injuries like whiplash and compression, and signs of spinal injury like pain, numbness, and deformity. It outlines steps for cervical spine immobilization, rapid extrication, helmet removal, and immobilizing a child in or out of a car seat.