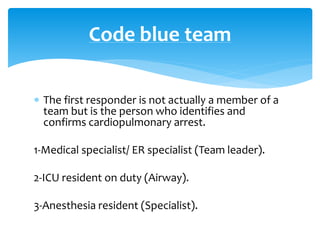
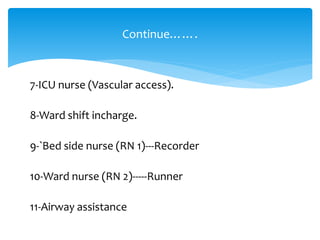
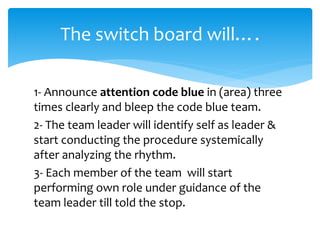
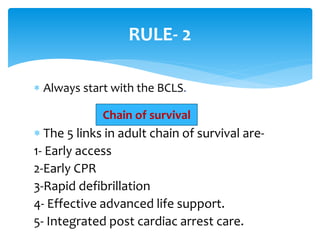
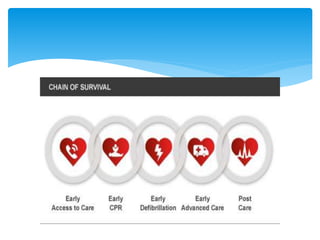
The document provides information about code blue procedures in a hospital setting. It defines a code blue as a medical emergency called when a patient experiences cardiopulmonary arrest. It outlines the roles and responsibilities of the code blue team members who respond. The procedures for initiating a code, performing CPR, documenting the event, and administering appropriate drugs to treat shockable and non-shockable cardiac rhythms are described.