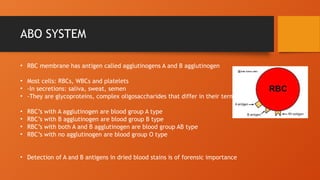
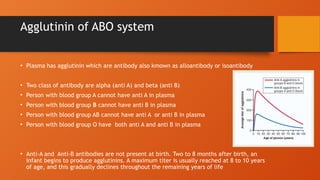
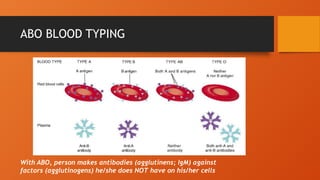
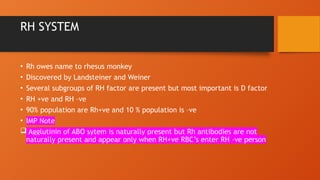
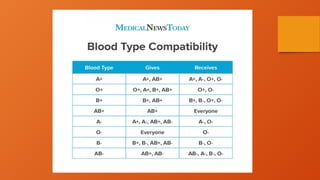
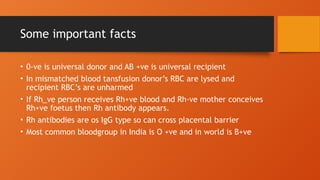
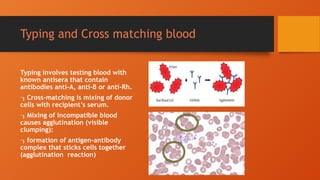
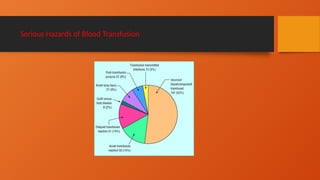
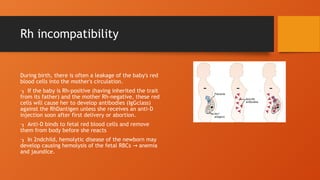
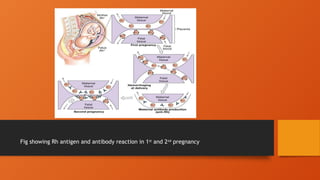
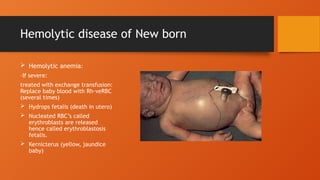
The document discusses blood groups, transfusion, and hemorrhage management, highlighting the ABO and Rh blood group systems. It explains blood typing, agglutinins, and potential transfusion reactions, emphasizing the importance of compatibility in transfusions and risks of incompatible blood. Additionally, it addresses hemolytic disease of the newborn and preventive measures for Rh incompatibility.