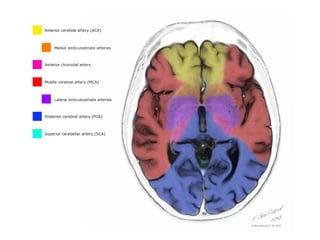
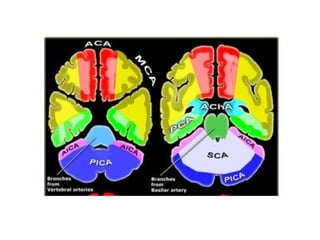
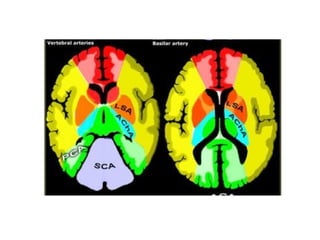
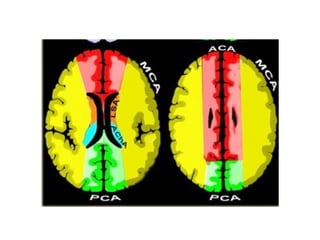
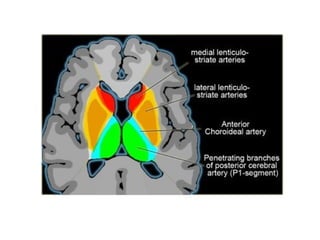
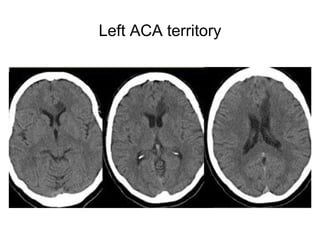
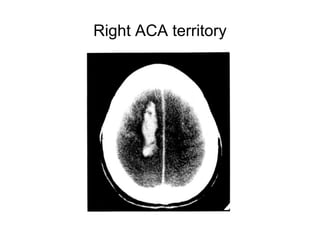
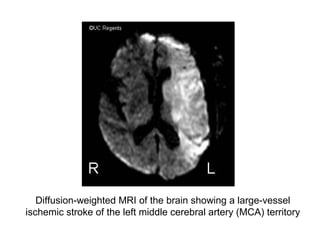
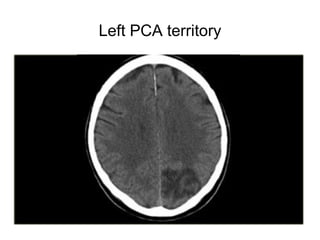
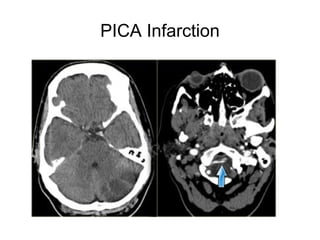
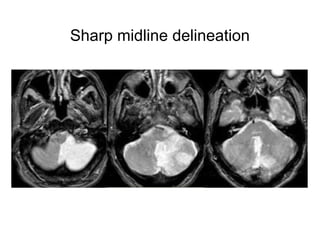
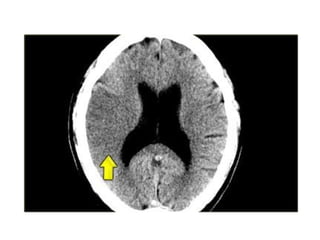
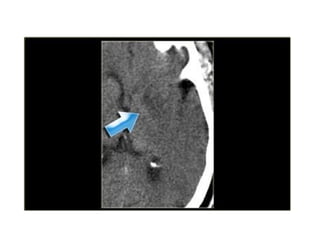
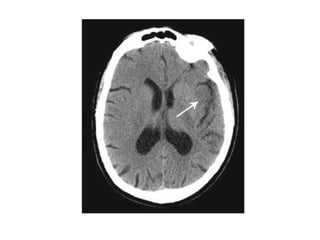
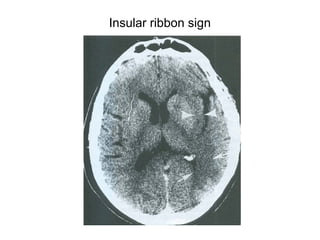
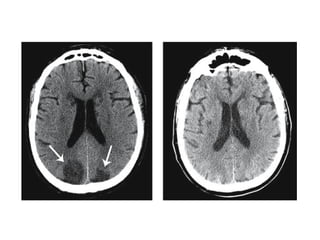
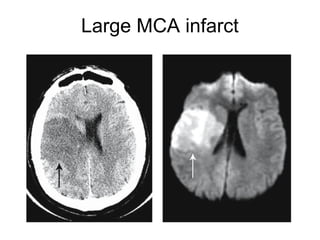
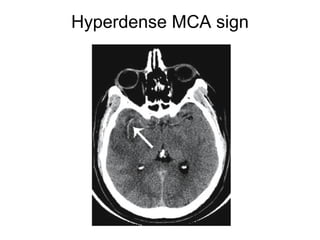
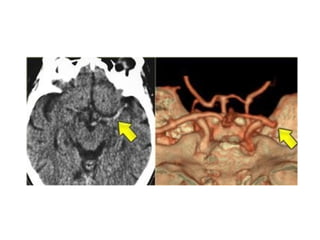
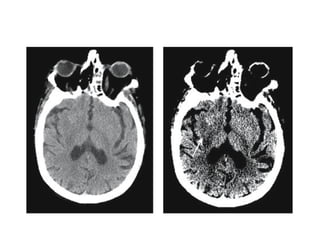
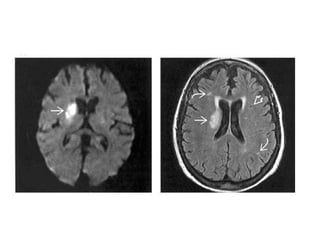
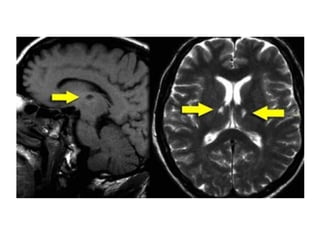
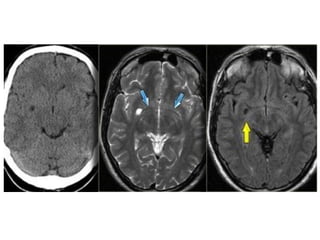
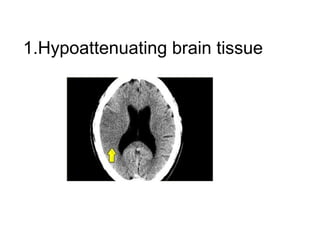
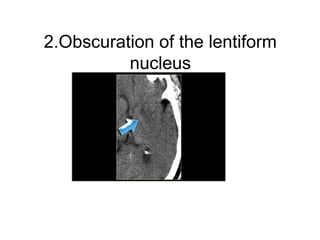
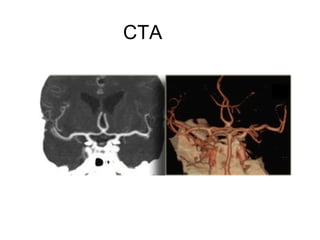
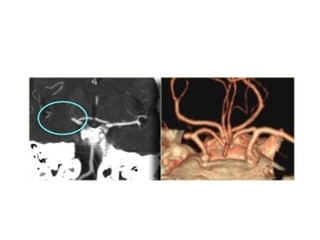
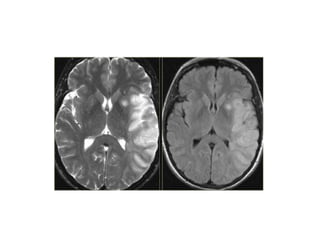
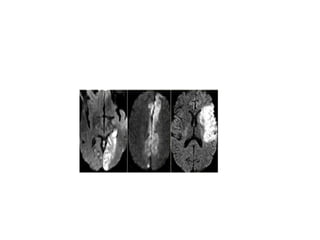
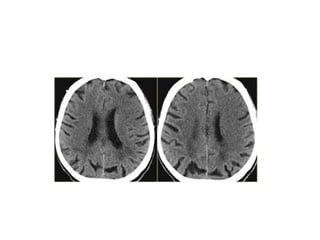
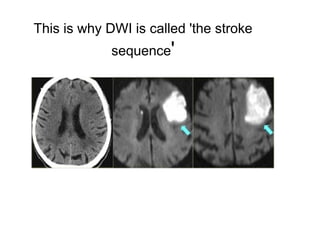
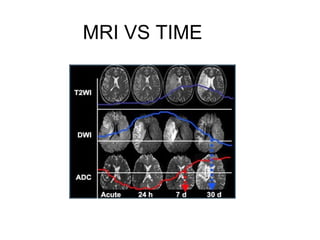
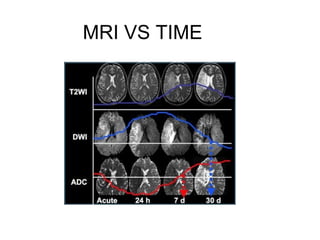
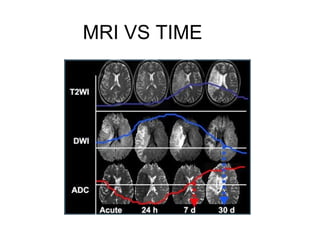
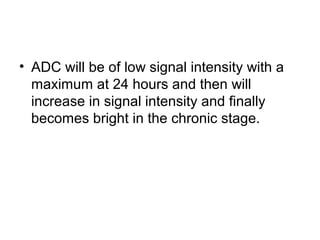
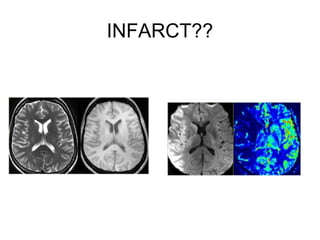
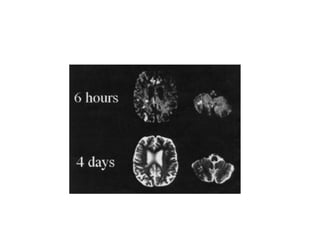
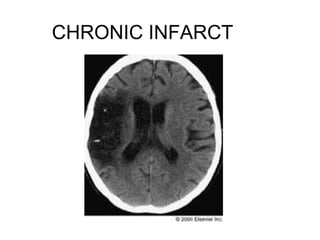
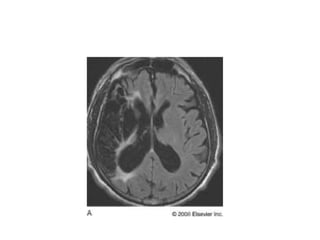
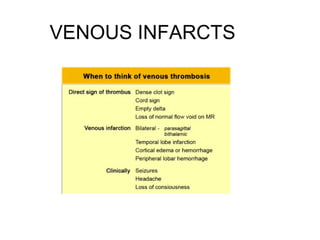
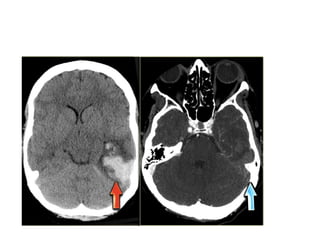
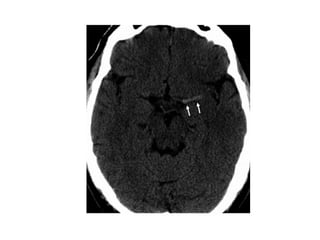
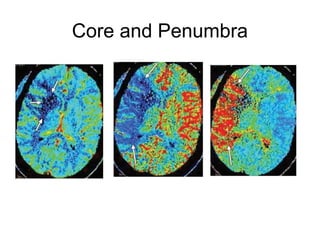
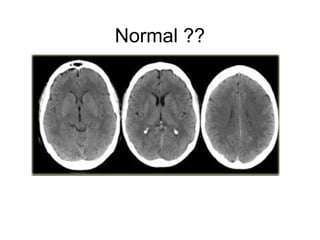
This document provides an overview of imaging in acute stroke, including CT and MRI. CT is often the initial imaging modality used to rule out hemorrhage. Early CT signs of infarction include hypodensity, obscuration of the lentiform nucleus, and the insular ribbon sign. Diffusion-weighted MRI is the most sensitive sequence for detecting acute ischemia. MRI can identify irreversibly injured tissue as well as potentially salvageable penumbral tissue. CT and MR angiography can detect vessel occlusions. CT perfusion can identify regions of low blood flow and volume that are at risk of infarction. The document reviews imaging findings over time and discusses venous infarcts.