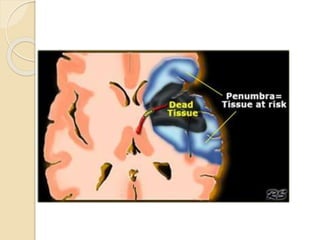
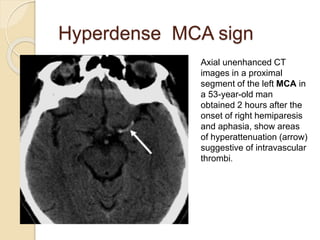
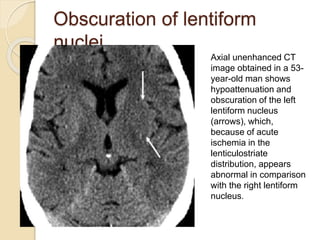
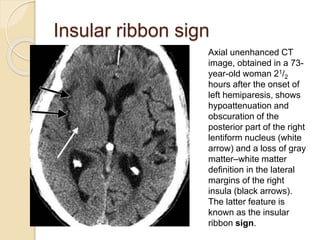
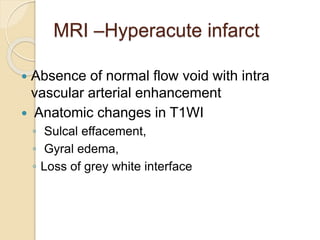
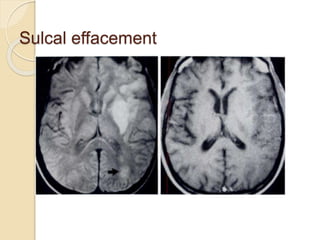
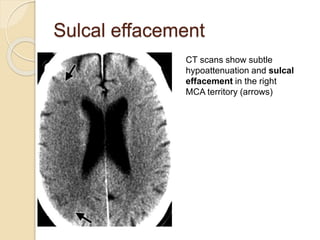
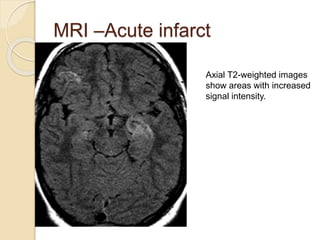
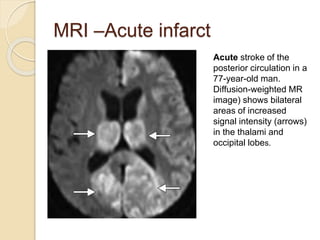
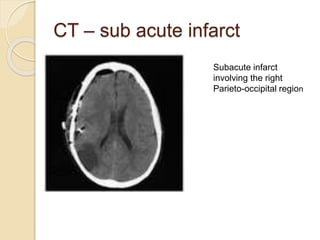
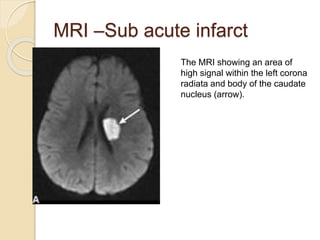
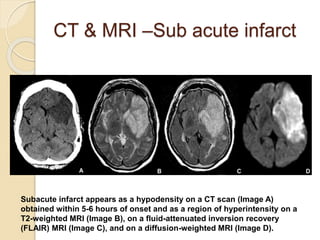
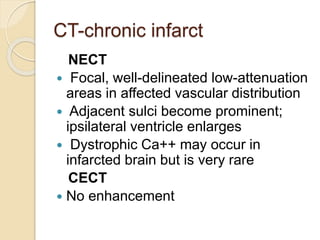
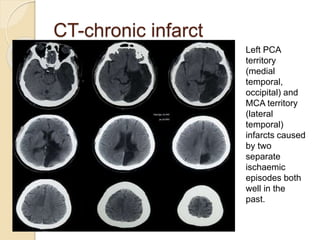
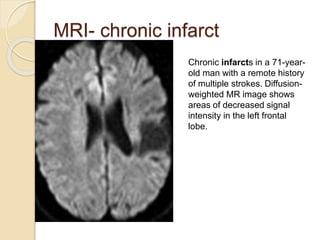
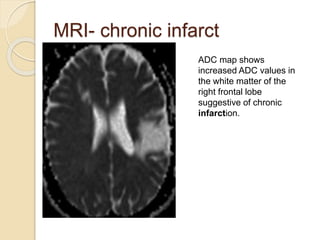
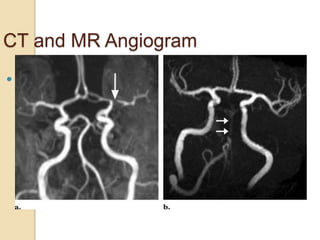
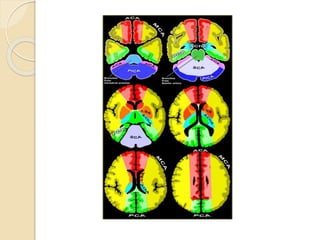
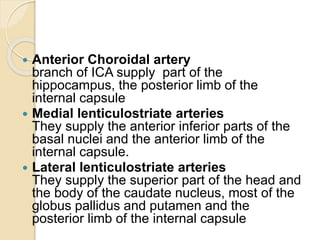
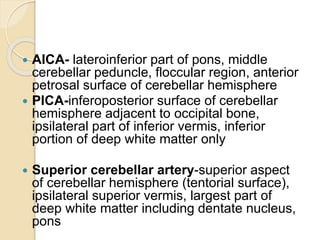
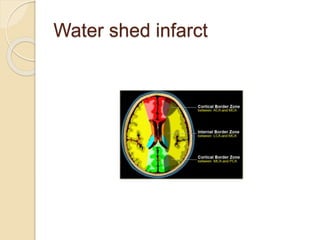
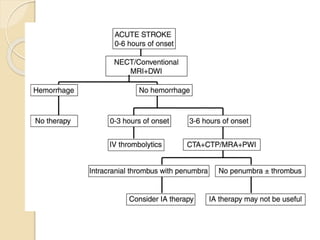
The document discusses cerebral infarcts, focusing on the pathophysiology of both global and focal ischemia, and the impact on various brain regions. It details the different imaging modalities used for diagnosis, including CT and MRI, as well as classification of infarcts based on their timing and characteristics. Additionally, it addresses the therapy considerations aimed at rescuing at-risk cells and descriptions of acute, subacute, and chronic infarcts, along with relevant anatomical and vascular territories supplied by major cerebral arteries.