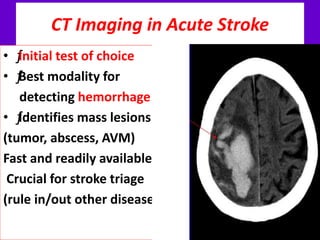
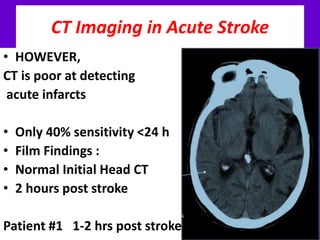
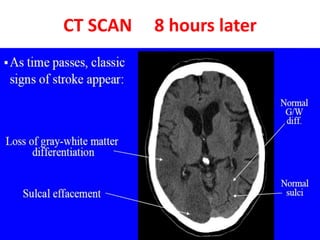
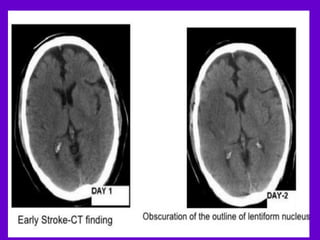
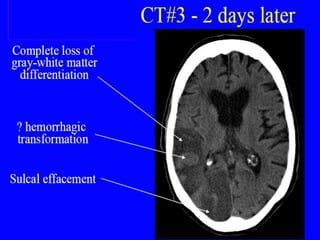
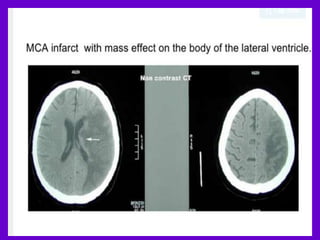
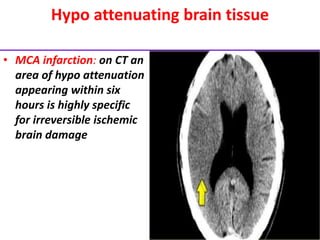
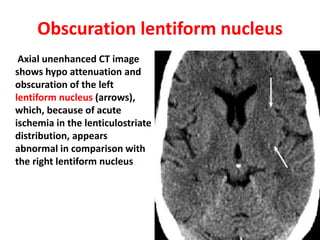
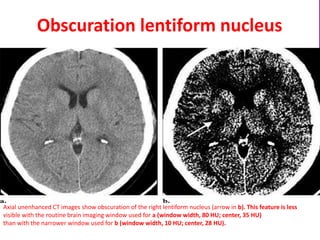
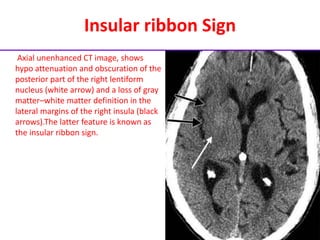
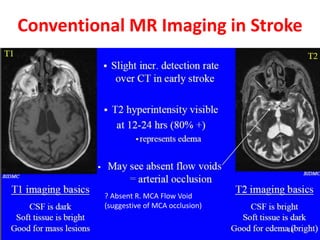
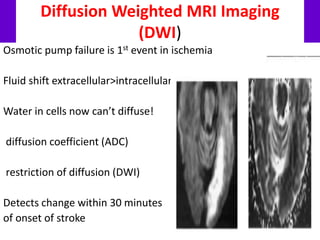
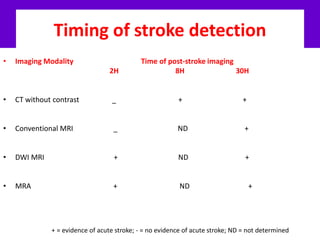
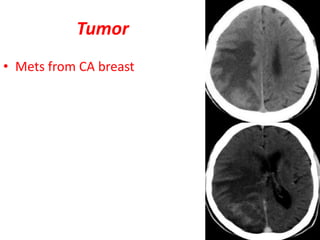
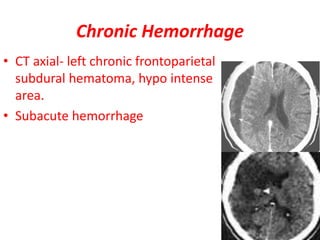
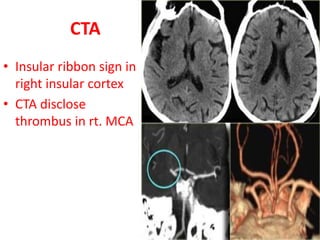
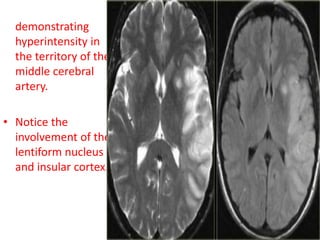
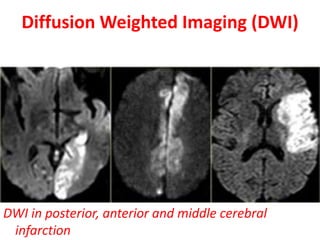
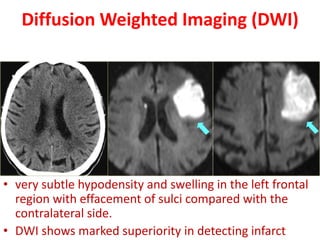
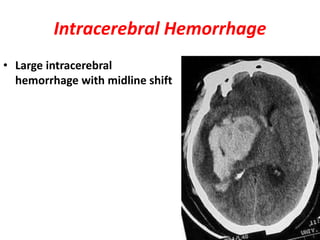
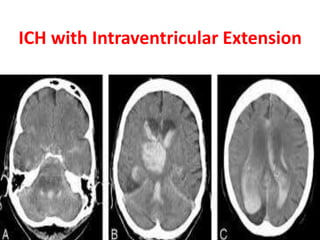
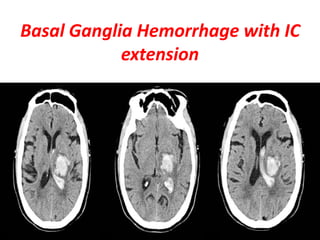
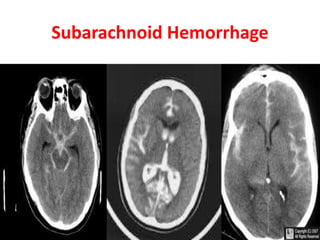
This document discusses imaging techniques for diagnosing strokes. It notes that CT scans are the initial test but can miss acute infarcts in up to 40% of cases within 24 hours. Diffusion-weighted MRI can detect strokes within 30 minutes and is more sensitive than CT for early detection. Perfusion imaging provides information on tissue at risk. The document reviews signs of acute infarction on CT and MRI appearances of different stroke types and hemorrhages. It emphasizes the importance of rapidly diagnosing strokes to determine treatment.