The document discusses upper gastrointestinal bleeding, including its definition, causes, risk factors, diagnosis, and management. Some key points:
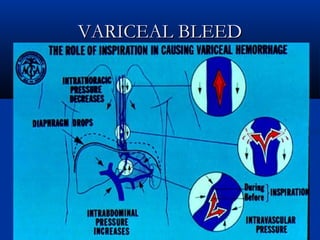
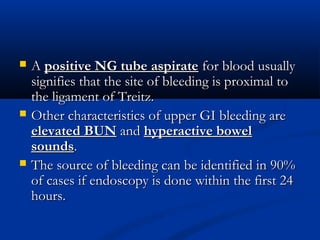
- Upper GI bleeding is defined as bleeding above the ligament of Treitz in the duodenum. Common causes include peptic ulcers, esophageal varices, and gastritis.
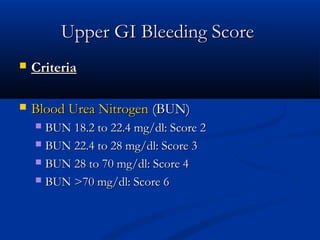
- Risk factors include NSAID/aspirin use, H. pylori infection, and older age. Endoscopy within 24 hours can identify the bleeding source in 90% of cases.
- Initial management involves nasogastric aspiration, IV fluids, blood transfusions, and endoscopy for high risk patients. Terlipressin or octreotide can help control var



























![ESOPHAGEAL VARICESESOPHAGEAL VARICES
I.I. Vasoconstrictors (somatostatin, octreotide,Vasoconstrictors (somatostatin, octreotide,
terlipressin) iv terlipressin infusion at 2 mg 6terlipressin) iv terlipressin infusion at 2 mg 6thth
hourly, generalized vasoconstriction leading tohourly, generalized vasoconstriction leading to
decreased blood flow to venous system.decreased blood flow to venous system.
II.II. Baloon tamponade – Triple lumen or FourBaloon tamponade – Triple lumen or Four
lumen tube with esophageal and gastric balloons.lumen tube with esophageal and gastric balloons.
(Always intubate the patient prior to this(Always intubate the patient prior to this
procedure to prevent aspiration)procedure to prevent aspiration)
III.III. Endoscopic variceal liagation[Band ligation]Endoscopic variceal liagation[Band ligation]
IV.IV. SclerotherapySclerotherapy
V.V. Antibiotic therapyAntibiotic therapy](https://image.slidesharecdn.com/uppergibleed-160515041855/85/Upper-gi-bleed-31-320.jpg)