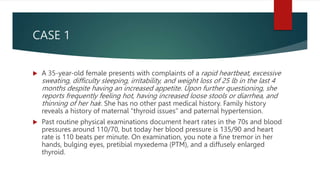
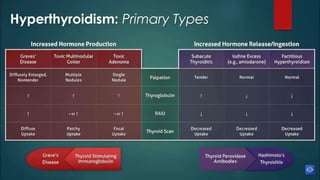
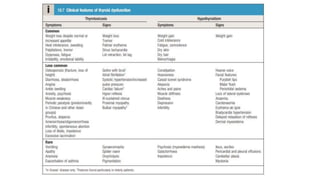
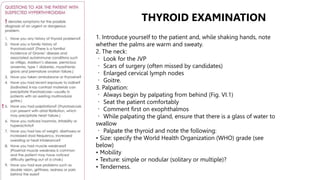
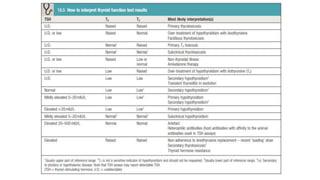
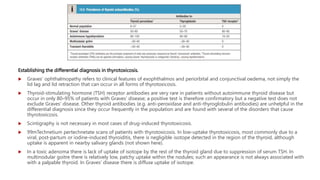
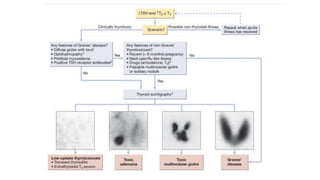
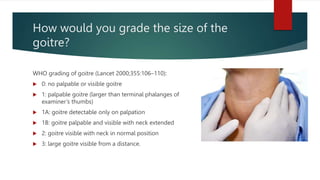
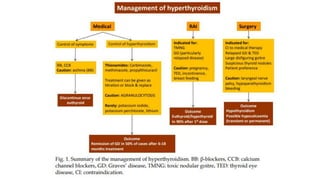
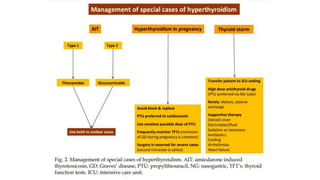
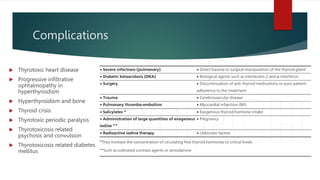
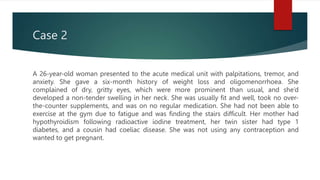
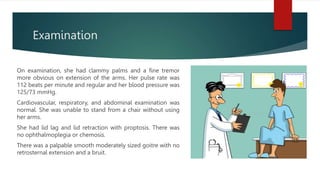
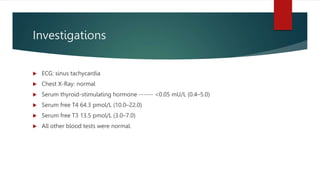
The document presents two cases of hyperthyroidism, emphasizing symptoms such as rapid heartbeat, weight loss, and goiter, leading to a diagnosis of Graves' disease. It outlines the examination methods for thyroid abnormalities and discusses the necessary differential diagnosis and treatment options. Additionally, it covers the importance of screening patients with various risk factors for thyroid dysfunction.