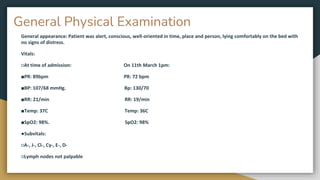
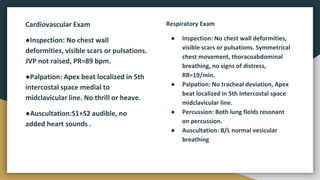
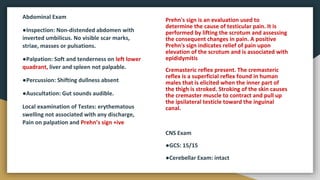
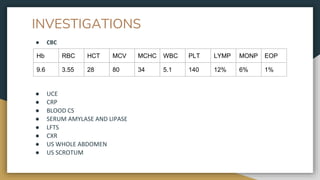
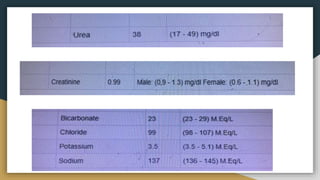
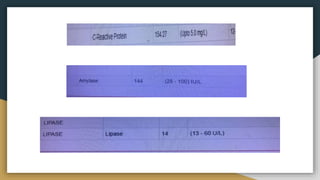
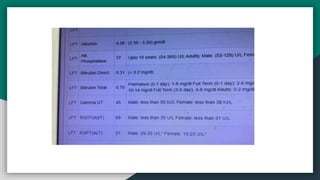
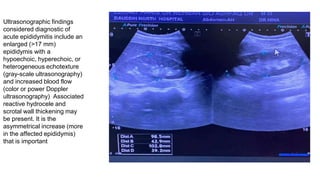
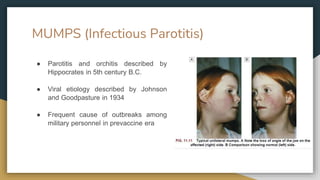
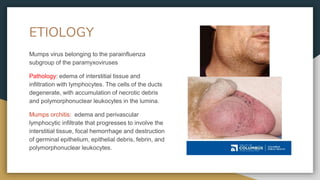
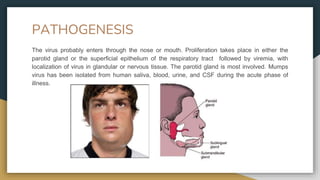
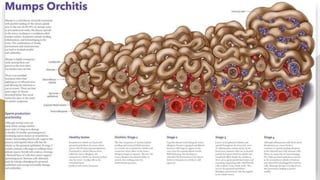
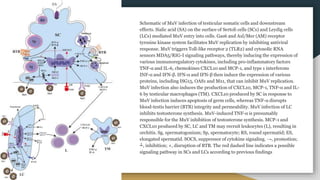
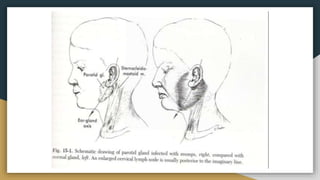
Samina Hussain presented a case of a 33-year-old male who presented to the emergency room with complaints of testicular swelling for 3 days and fever for 3 days. On examination, he was found to have erythematous swelling of the left testis with tenderness and a positive Prehn's sign. Ultrasound showed an enlarged epididymis. He was diagnosed with acute epididymitis and started on IV hydration, antibiotics, and analgesics. Mumps and resulting orchitis were discussed as a possible cause.