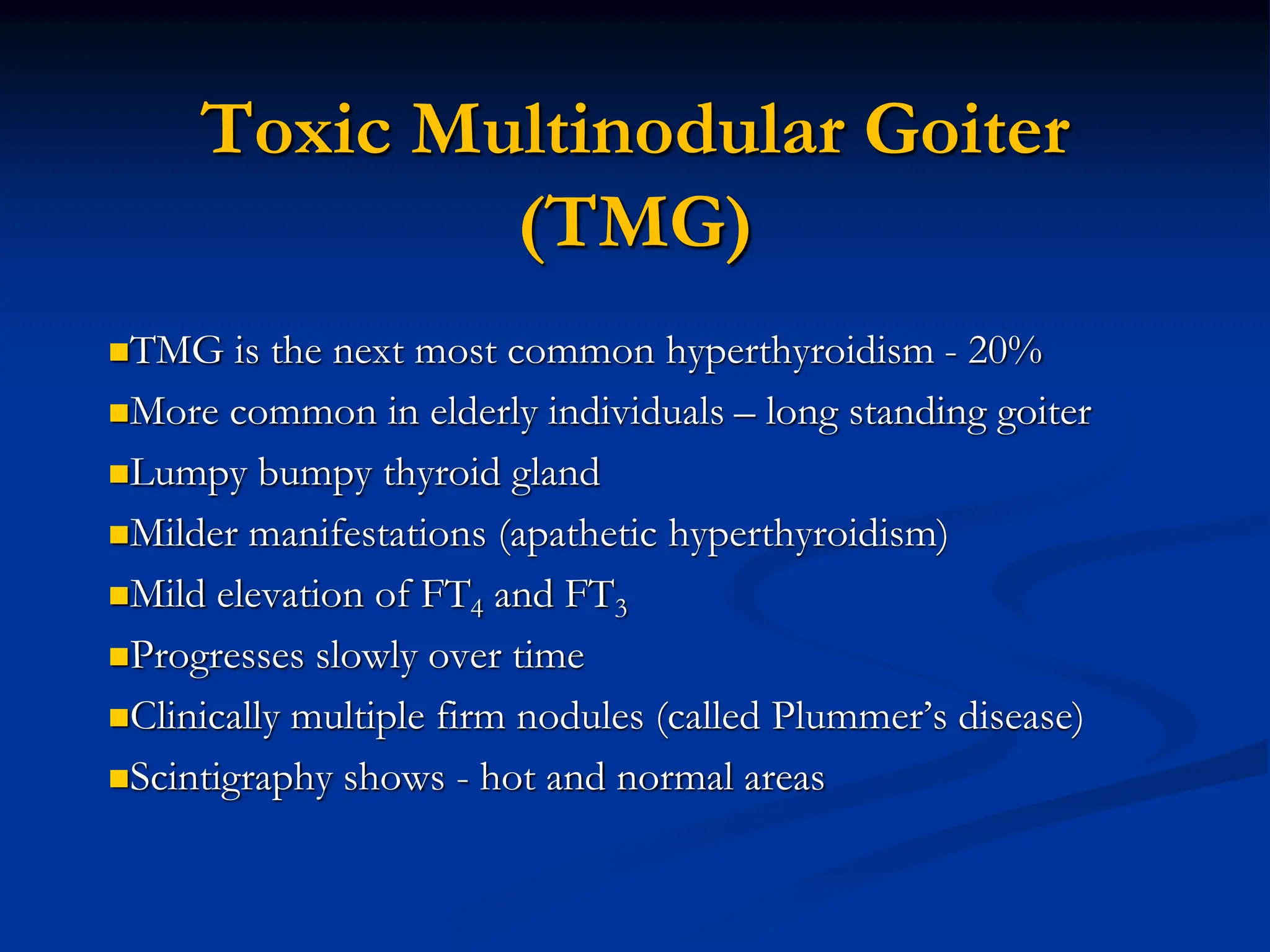
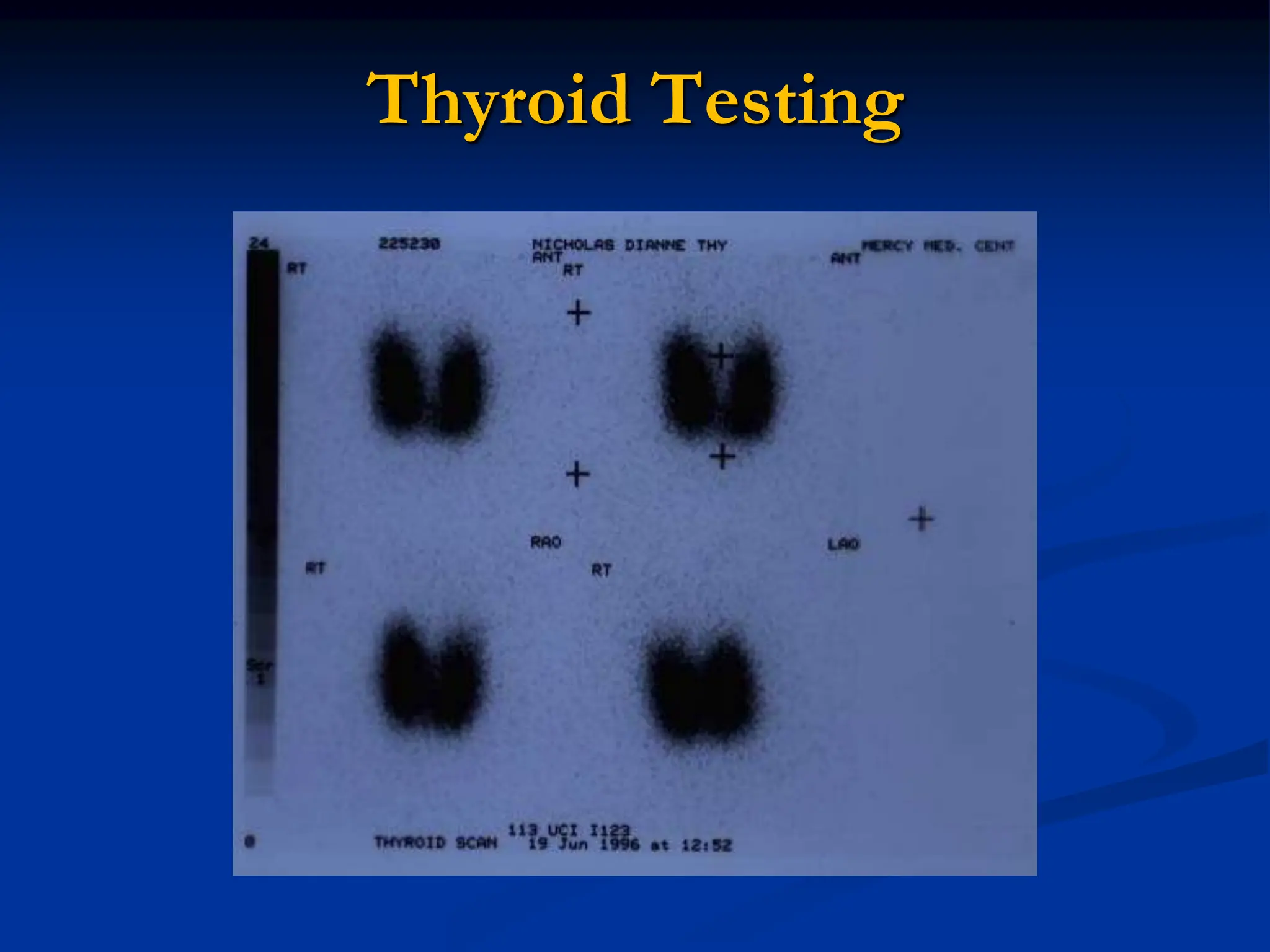
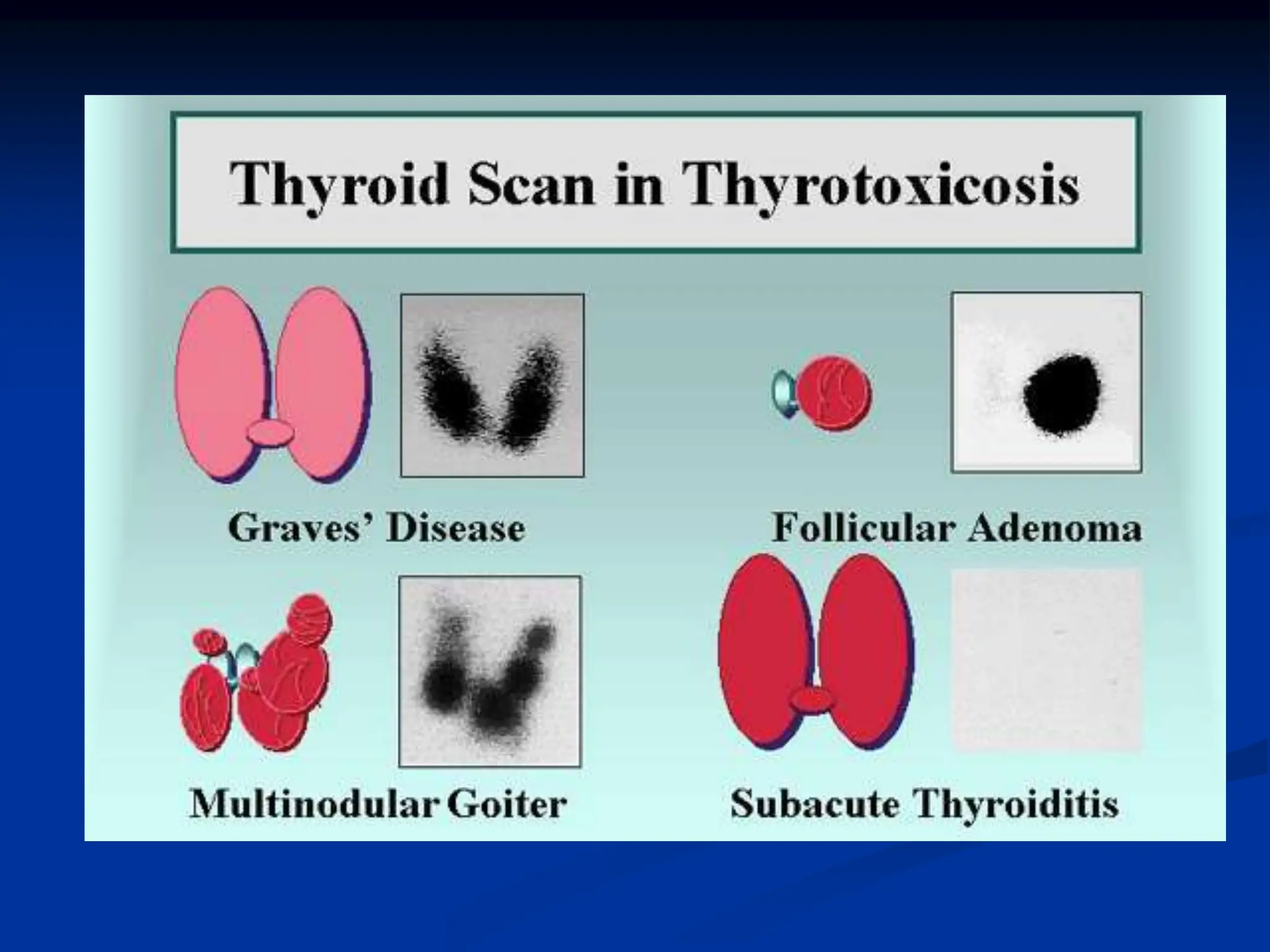
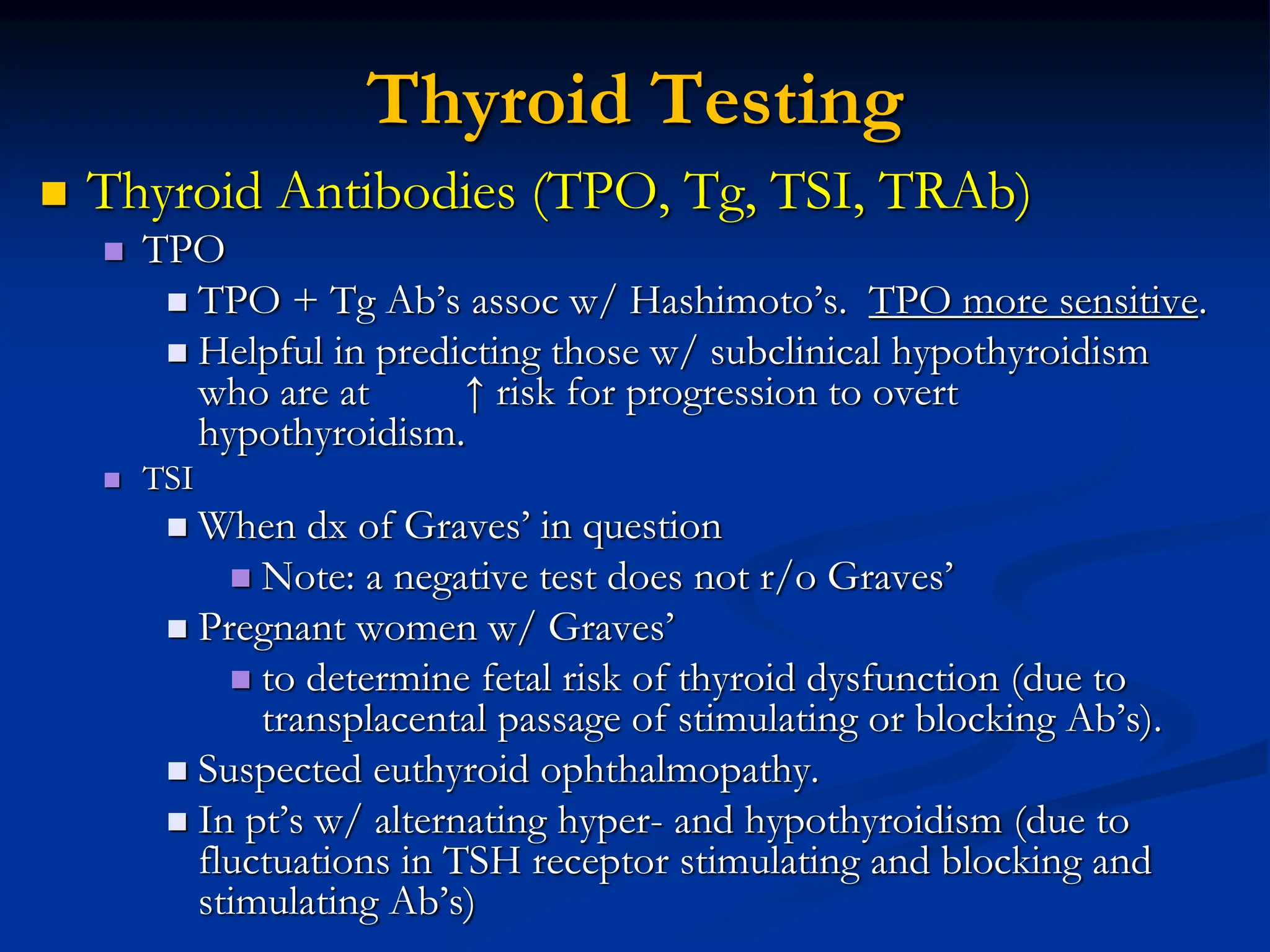
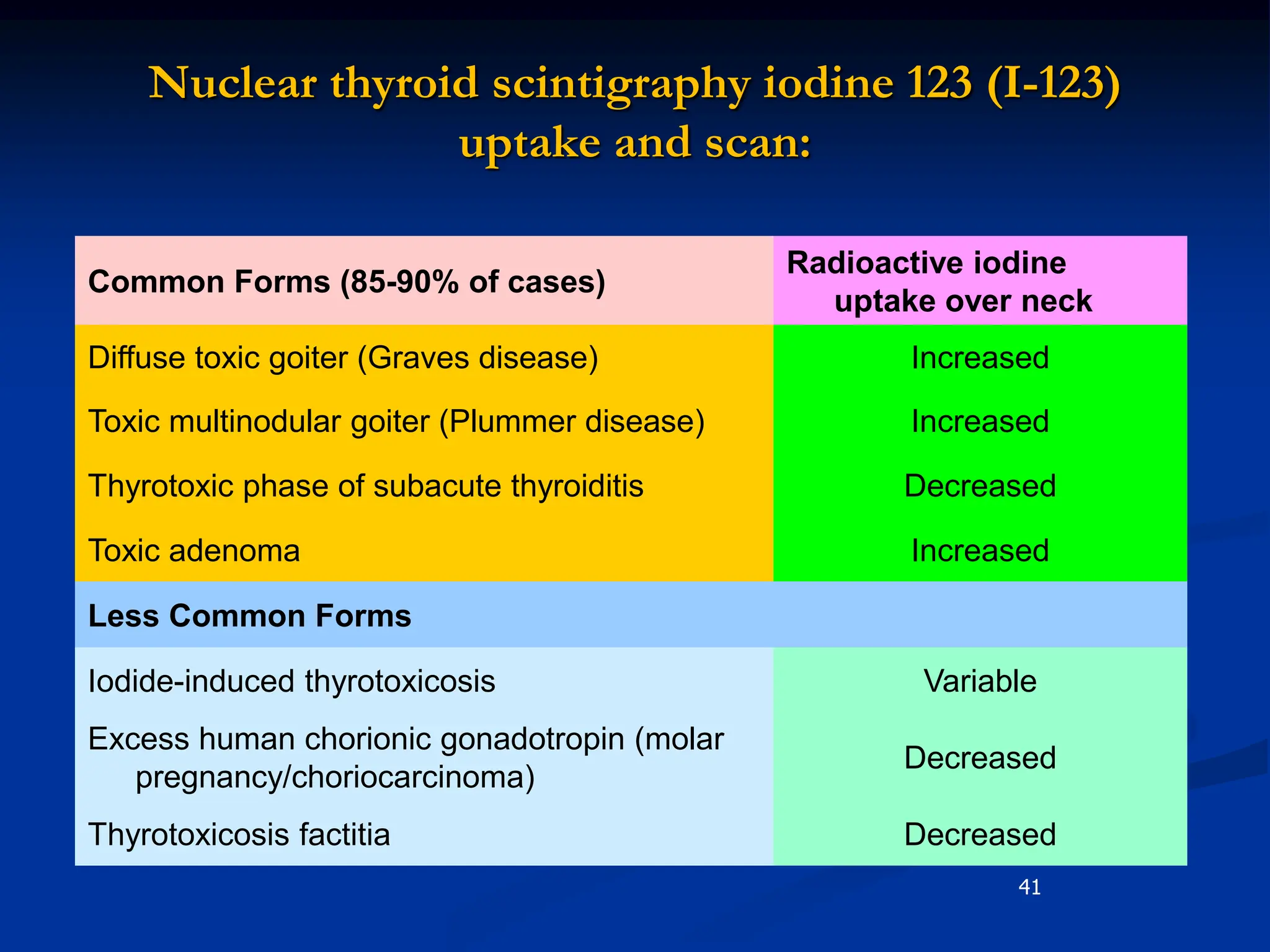
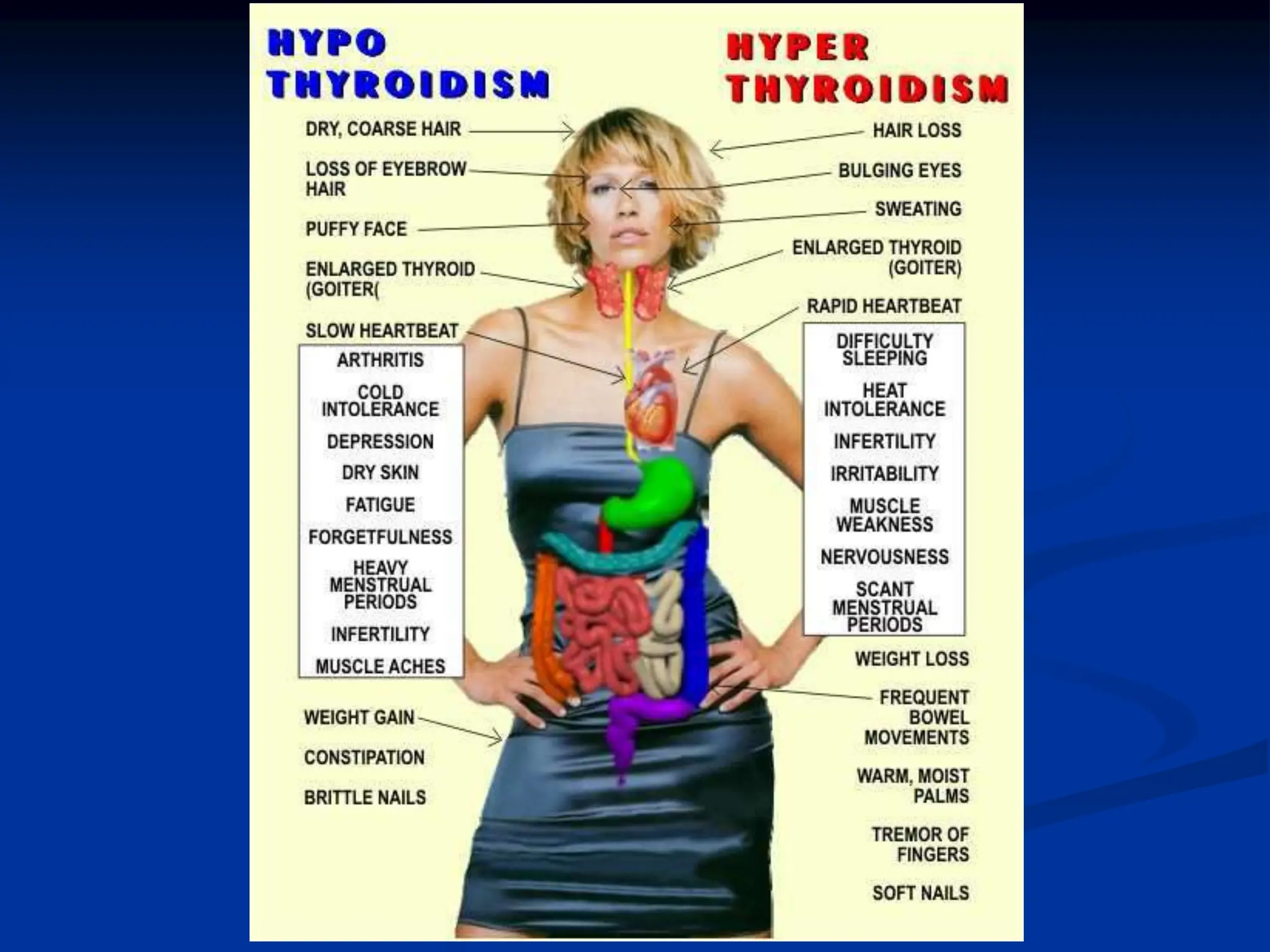
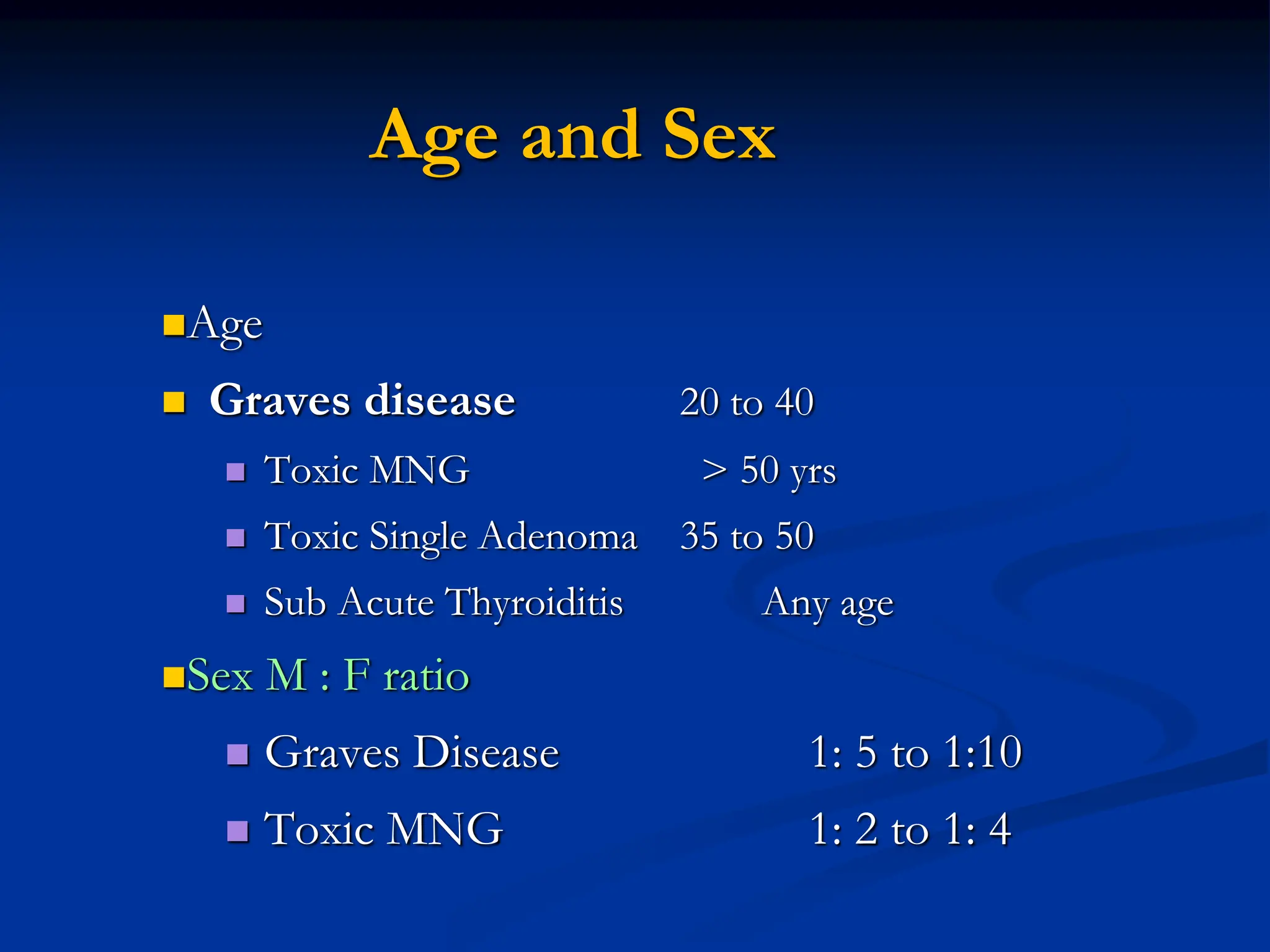
The document provides an extensive overview of hyperthyroidism and thyrotoxicosis, discussing its prevalence, causes, and treatments. Key conditions included are Graves' disease, toxic multinodular goiter, and subacute thyroiditis, with symptoms and diagnostic methods outlined. The text emphasizes the importance of understanding the various causes of hyperthyroidism to tailor appropriate treatment strategies.