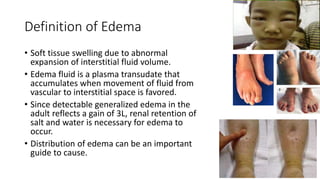
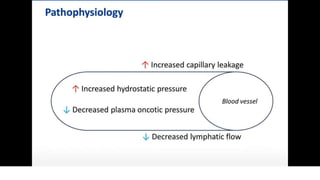
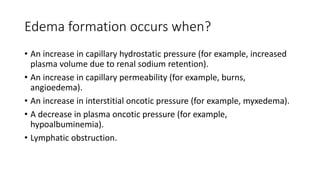
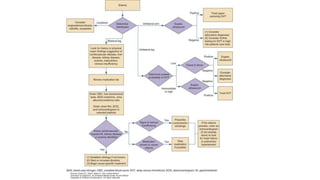
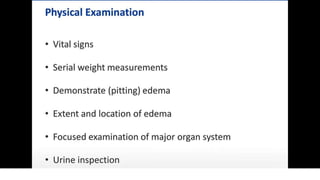
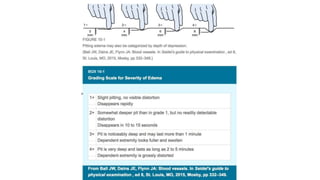
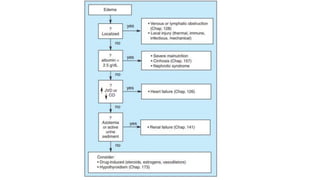
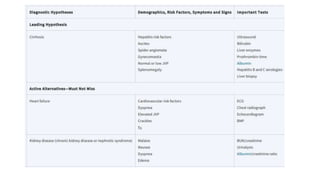
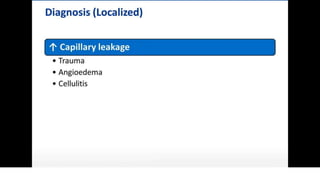
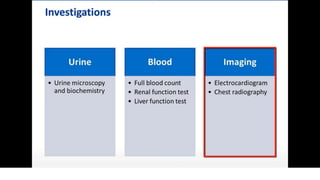
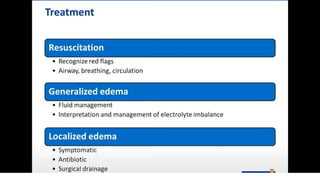
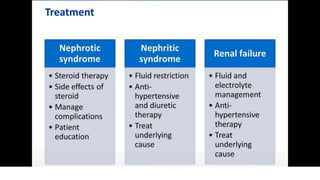
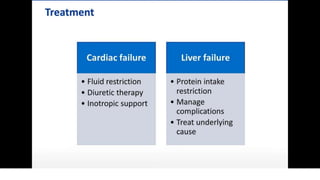
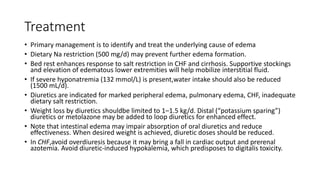
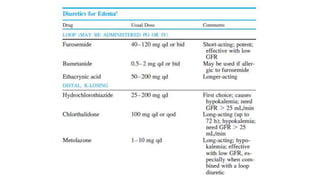
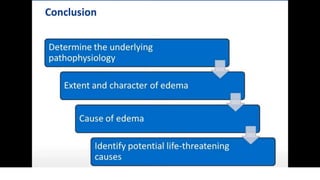
The document outlines edema as a condition characterized by swelling due to the accumulation of interstitial fluid, triggered by factors such as increased capillary pressure or permeability, and lymphatic obstruction. Treatment focuses on addressing the underlying causes, dietary restrictions, supportive measures, and appropriate use of diuretics while monitoring for potential complications. Key points include careful management of fluid intake, especially in cases of severe hyponatremia, and the risks associated with overdiuresis in congestive heart failure.