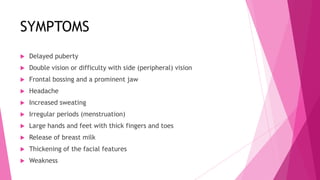
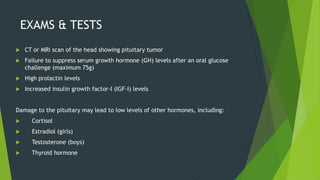
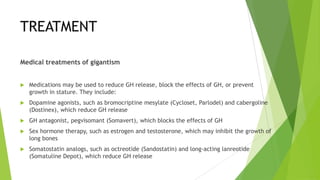
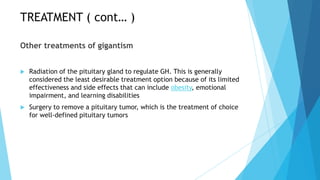
Acromegaly and gigantism are chronic metabolic disorders caused by excessive growth hormone levels. Acromegaly occurs in adulthood after bone growth plates have closed, causing tissue enlargement. Gigantism occurs in childhood before plate closure, resulting in abnormally large growth. Both are usually due to noncancerous pituitary tumors that overproduce growth hormone, leading to increased insulin-like growth factor levels and symptoms like enlarged hands, feet and head. Diagnosis involves blood tests and imaging to identify the source of excess growth hormone. Treatment focuses on surgery, radiation or medications to reduce hormone levels and stop further growth.