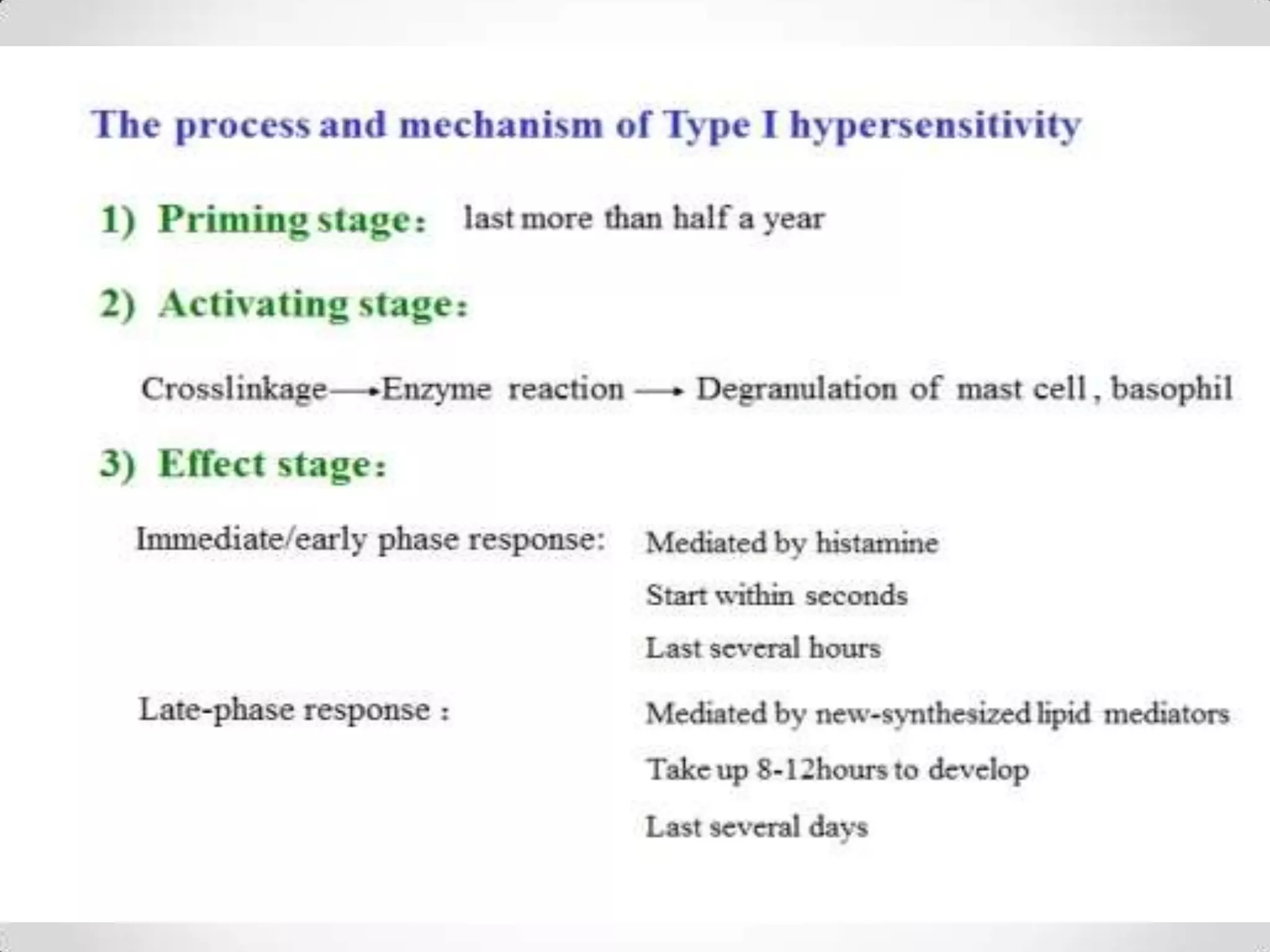
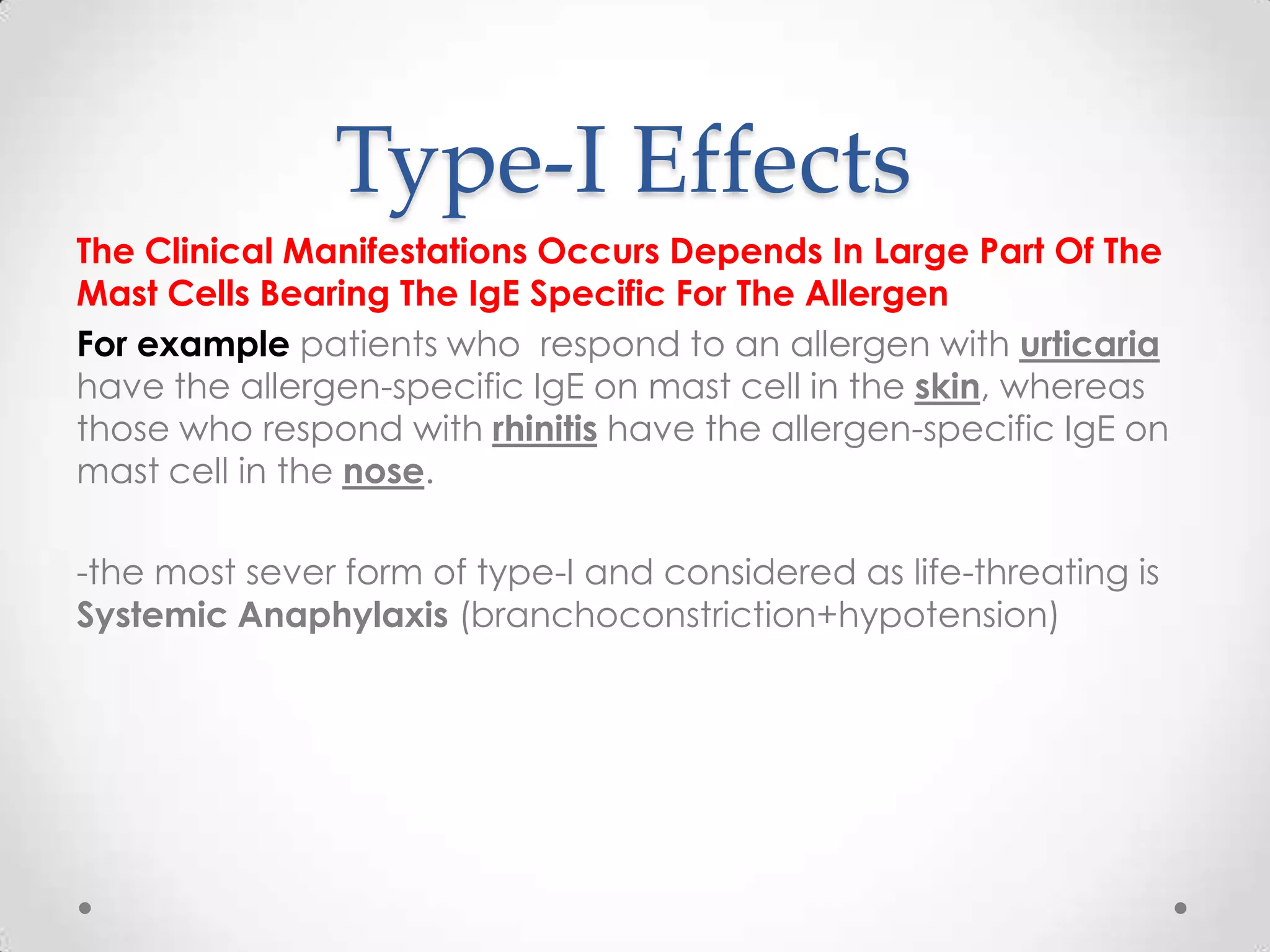
The document discusses hypersensitivity reactions, specifically focusing on type-I allergies which are characterized by an exaggerated immune response leading to tissue damage and symptoms like anaphylaxis. It outlines the mechanisms behind these reactions, the role of various mediators released from mast cells, and the clinical manifestations associated with allergies. Additionally, it addresses atopy as a genetic predisposition to produce excessive IgE and highlights diagnostic methods and treatment options.





![Type [I]
About:
-This type is the most common one.
-Called Immediate hypersensitivity and anaphylactic hypersensitivity as
well.
-This type doesn’t occur in all population.
-symptoms of this type are called : anaphylaxis
KEYS
1-Mast Cell
A Large cell which contains granules or vesicles containing Mediators like
Histamine Inside it ,and it’s role related to allergy .
2-Allergen : is a type of antigen that produces an
abnormally immune response.
3-IgE : Is a specific one of the 5 antibodies which plays an
essential role in allergy type-I,And it’s induced by this allergen, produced by
B-cells.](https://image.slidesharecdn.com/hypersensitivityrania1-140217133125-phpapp02/75/Hypersensitivity-Or-Allergy-6-2048.jpg)



![Mechanism [Con’t]
*What are the mediator that released from mast cell?
Mediator are soluble substances which cause manifestation of
disease.
Calcium and cyclic nucleotide play role in release of these mediators
Note : NO Single mediator accounts or causes for all the allergy
Type-I Manifestation or symptoms.
*There are 3 classes of mediators derived from mast
cell :
1-Preformed or primary Mediators
2-Newly sensitized ,synthesized or Secondary
Mediators
3-cytokines and chemokines.](https://image.slidesharecdn.com/hypersensitivityrania1-140217133125-phpapp02/75/Hypersensitivity-Or-Allergy-12-2048.jpg)



![[Con’t]
Effects of these substances when released
1-Histamine: vasodilation, increased capillary
permeability & smooth-muscle contraction.
Clinically : rhinitis (hay fever) urticaria and
angioedema can occur and bronchospasm.](https://image.slidesharecdn.com/hypersensitivityrania1-140217133125-phpapp02/75/Hypersensitivity-Or-Allergy-18-2048.jpg)
![[Con’t]
2-Release of Leukotrienes: the principal mediator in
the bronchoconstriction of asthma ,increased
vascular permeability and smooth muscle constriction
occur](https://image.slidesharecdn.com/hypersensitivityrania1-140217133125-phpapp02/75/Hypersensitivity-Or-Allergy-19-2048.jpg)
![[Con’t]
3-Eosinophil Chemotactic Factor Anaphylaxis (ECF-A)
-is a tetra peptide
-when released attracts Eosinophil's
-may reduce the severity of allergy type-I
-The role in Type-I is Uncertain
-they release histaminase and arylsulfatase which
degrade 2 important mediators, Histamine and SRS-A
(slow-reacting substances of anaphylaxis)respectively](https://image.slidesharecdn.com/hypersensitivityrania1-140217133125-phpapp02/75/Hypersensitivity-Or-Allergy-20-2048.jpg)
![[Con’t]
4-Serotonin(hydroxytryptamine)
When released causes increased vascular
permeabiltty,capillary dilation and smooth muscles
contraction.
5-prostaglandin and thromboxanes
-Prostaglandin causes dilation and increased
permeability and bronchoconstriction
-Thromboxanes aggregate platelets](https://image.slidesharecdn.com/hypersensitivityrania1-140217133125-phpapp02/75/Hypersensitivity-Or-Allergy-21-2048.jpg)