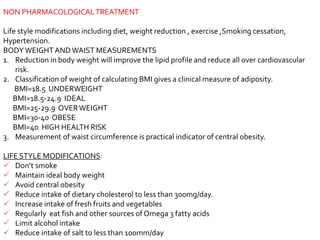
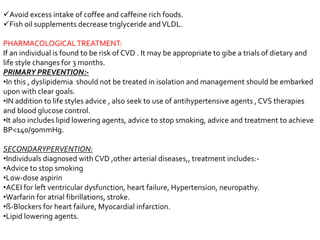
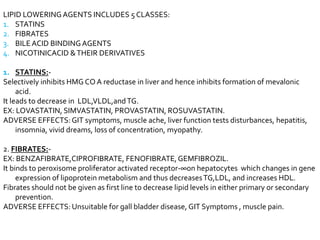
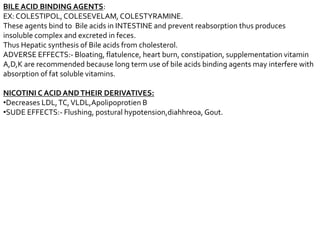
This document discusses dyslipidemia, which refers to abnormal levels of lipids in the blood such as elevated cholesterol, triglycerides, and low HDL. It causes by the accumulation of LDL cholesterol and leads to atherosclerosis and increased risk of heart disease. Treatment involves lifestyle modifications like diet, exercise, weight loss to lower lipid levels as well as lipid-lowering medications like statins which work by inhibiting cholesterol production in the liver. The goals of treatment are to lower LDL cholesterol and reduce risk of heart attacks and other cardiovascular events.