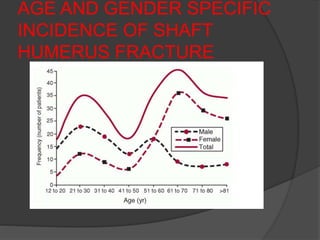
1) Fractures of the humeral shaft account for 3-5% of all fractures. They can often heal successfully with conservative treatment using splinting or bracing.
2) Operative treatment with plating or nailing is recommended for fractures that cannot be reduced or maintained non-operatively, open fractures, or those with neurovascular injuries.
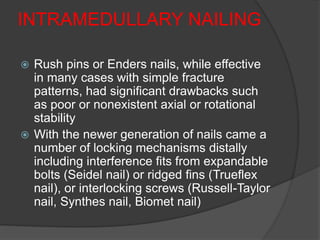
3) Plating remains the gold standard operative treatment, providing high union rates and rapid return to function. Intramedullary nailing is an alternative, especially for segmental or pathological fractures. Complications can include radial nerve palsy, malunion, and stiffness.



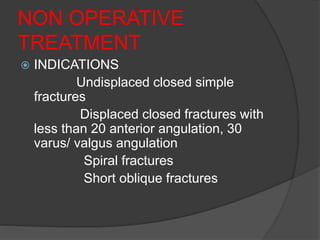


![CONTRAINDICATIONS
Lack of co-operation by the pt.
Bed-ridden & mentally incompetent pts.
Deficient sensibility of the limb [D.M with
P.N]
When the brace cannot fitted closely
and accurately.
Fractures of both bones forearm when
reduction is difficult.
Intraarticular fractures.](https://image.slidesharecdn.com/humerusfracture-150505172712-conversion-gate02/85/Humerus-fracture-39-320.jpg)