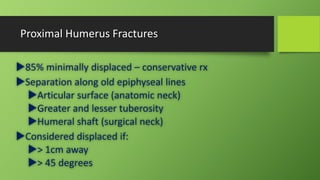
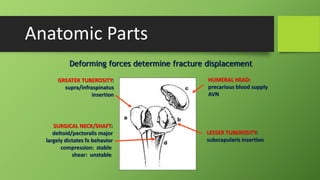
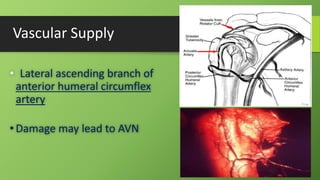
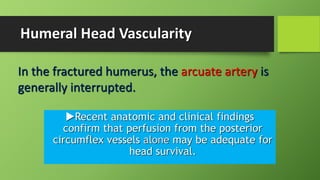
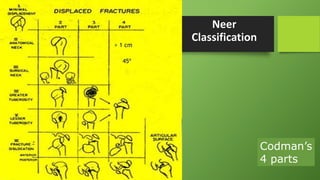
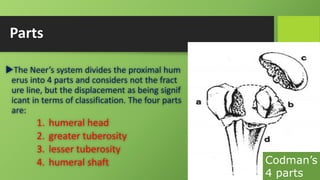
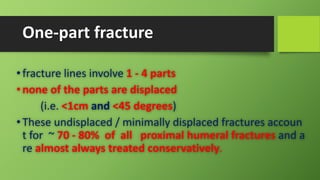
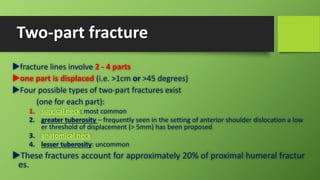
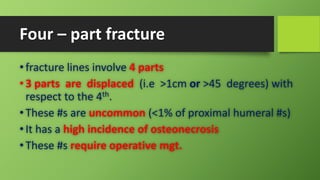
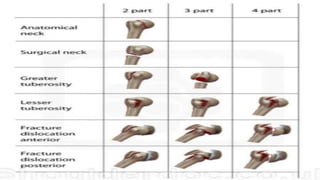
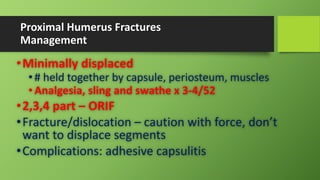
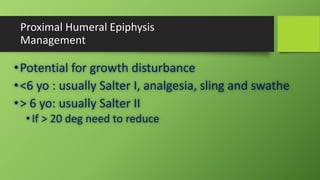
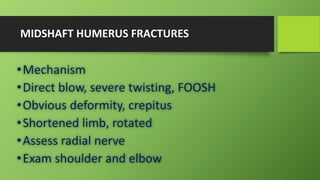
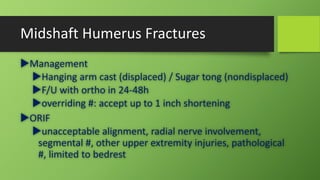
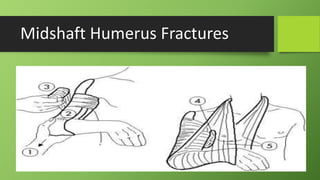
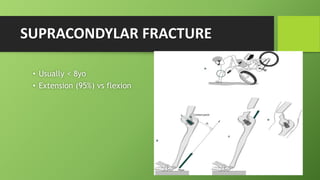
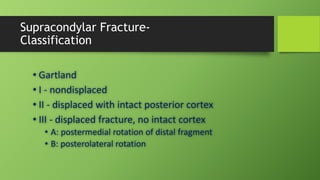
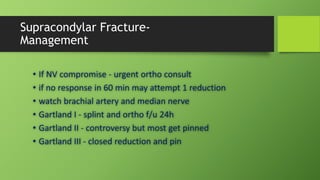
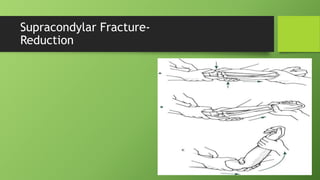
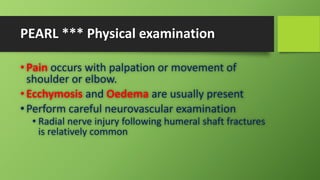
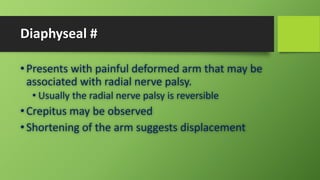
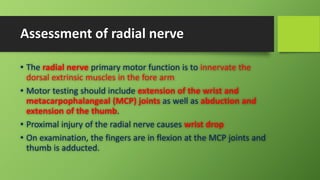
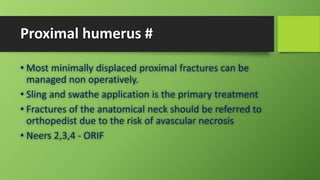
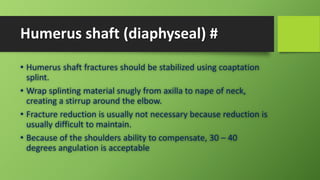
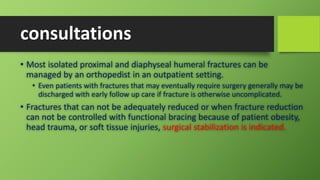
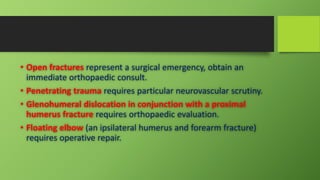
Fractures of the humerus can occur in the proximal, midshaft, or distal regions. Proximal humerus fractures make up the majority and are often minimally displaced, allowing for nonoperative treatment with sling immobilization. Displaced proximal fractures are classified using Neer's system and may require open reduction and internal fixation. Midshaft fractures can cause radial nerve palsies and often are treated with splinting, while displaced fractures may need surgery. Supracondylar fractures in children frequently involve the elbow and are the most common type of elbow fracture in young kids.