1) Fractures of the humerus shaft account for 3-5% of all fractures and usually heal well with conservative treatment.
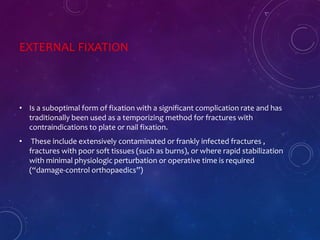
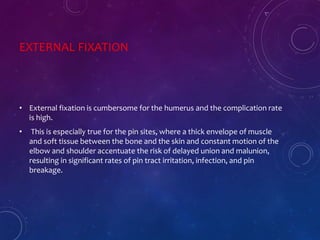
2) Non-operative treatment is indicated for undisplaced or minimally displaced fractures, while operative treatment involving plating or nailing is used for more displaced fractures or those with complications.
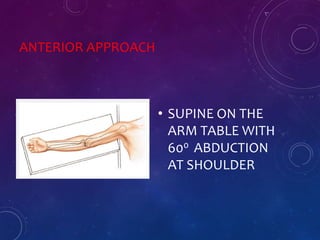
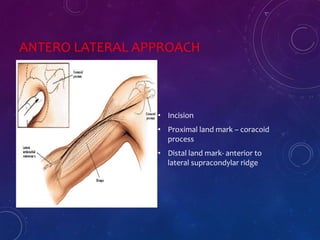
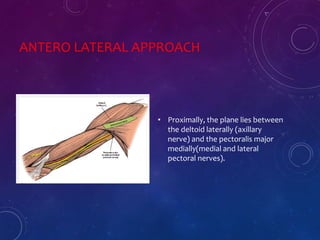
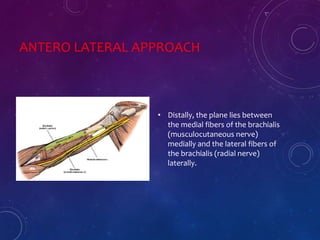
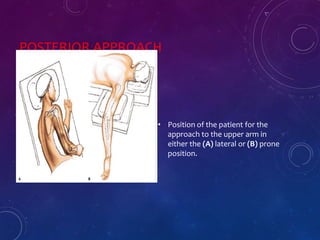
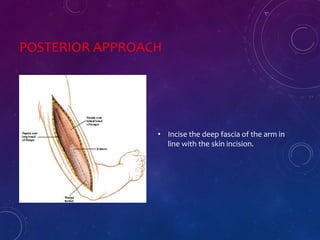
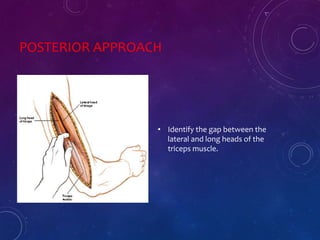
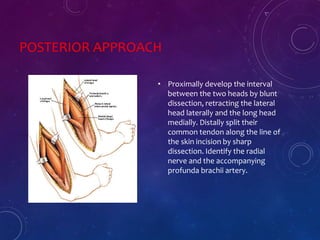
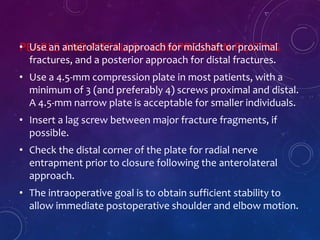
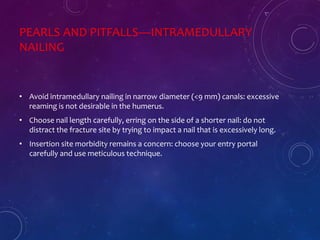
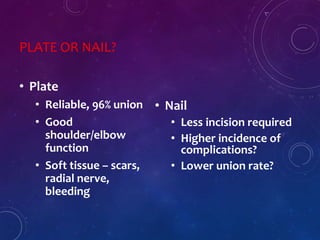
3) Surgical treatment options include plating through various approaches like anterior or posterior, as well as intramedullary nailing. Plating remains the gold standard due to high union rates and limited complications.









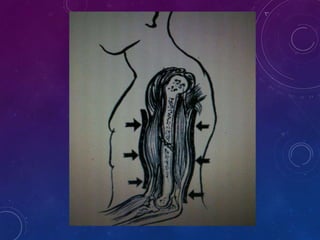
![CONTRAINDICATIONS
• Lack of co-operation by the pt.
• Bed-ridden & mentally incompetent pts.
• Deficient sensibility of the limb [D.M with P.N]
• When the brace cannot fitted closely and accurately.
• Fractures of both bones forearm when reduction is difficult.
• Intraarticular fractures.](https://image.slidesharecdn.com/humerusfracture-170427173809/85/Humerus-Shaft-fractures-PAWAN-44-320.jpg)