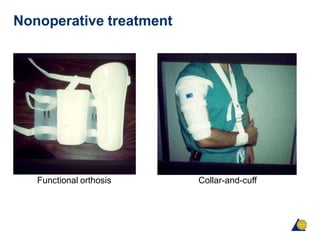
Humeral shaft fractures can often be treated nonoperatively with a functional brace, though some indications for surgery exist. Flexible nails and plates are common operative options, with plates preferred by some studies. Plates and nails have similar union rates, but nails are associated with more complications like shoulder discomfort. Immediate exploration is recommended for open fractures or distal spiral fractures due to higher risk of radial nerve injury.

![Humeral shaft fractures
• Humeral shaft fractures account for approximately 1–3%
of all fractures [Beaty 1996, Zuckerman, 1996]
• Usually the result of blunt trauma such as a fall or from
high-energy trauma including motor vehicle accidents
and gunshot injuries
• Fracture displacement is the result of muscular forces](https://image.slidesharecdn.com/humeralshaft-160422131313-220808083940-d7f47c79/85/humerus-shaft-3-320.jpg)