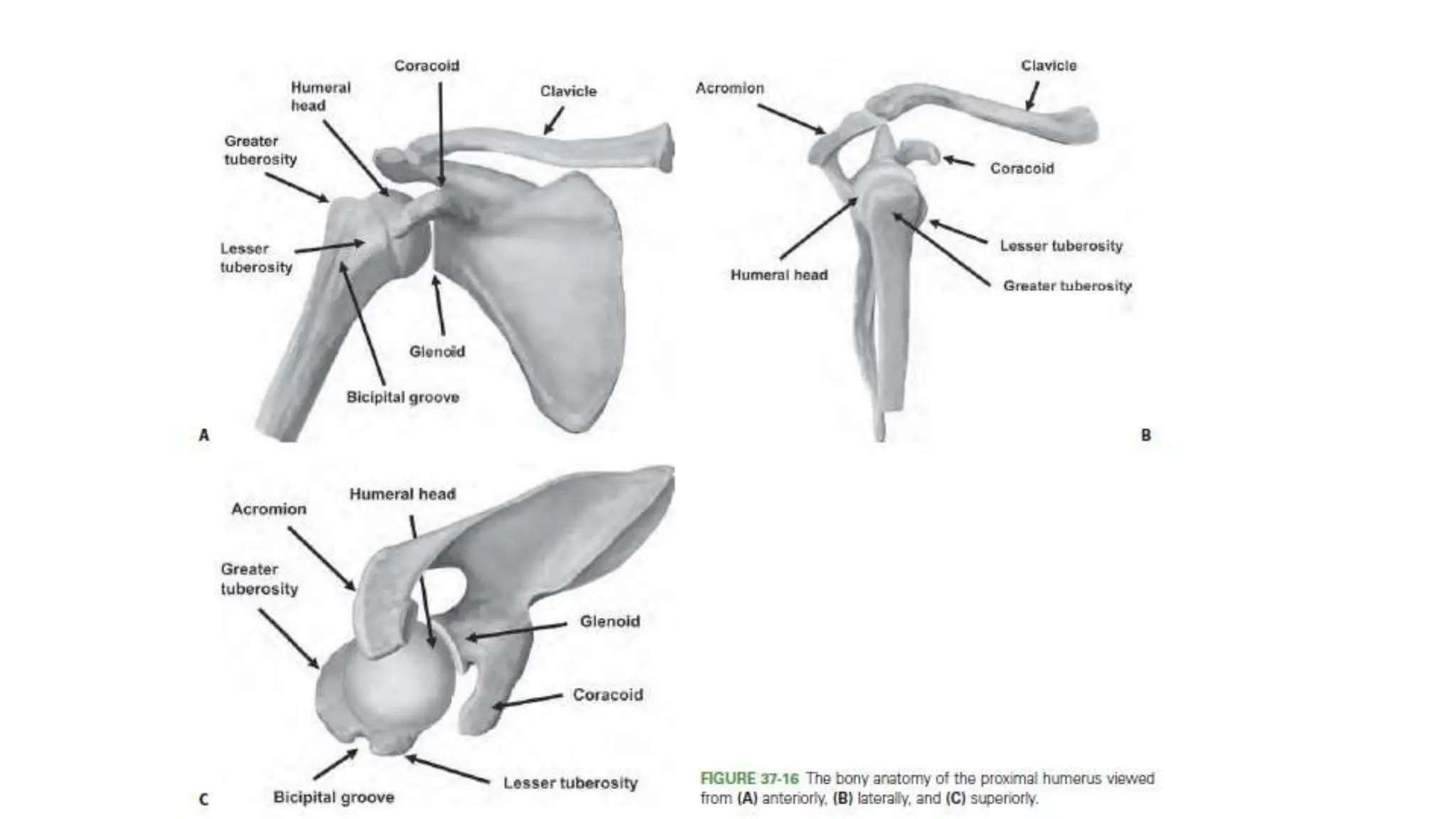
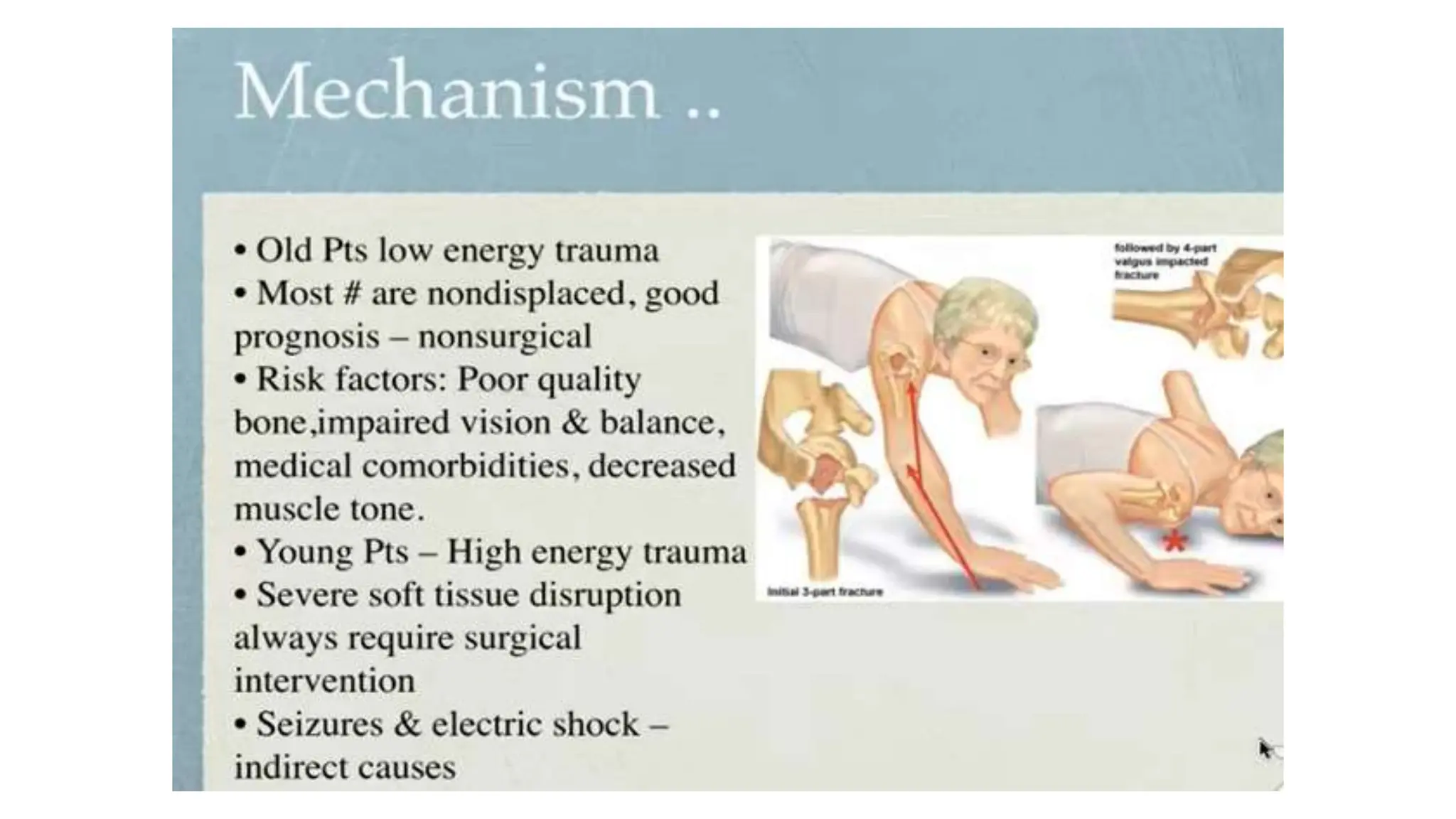
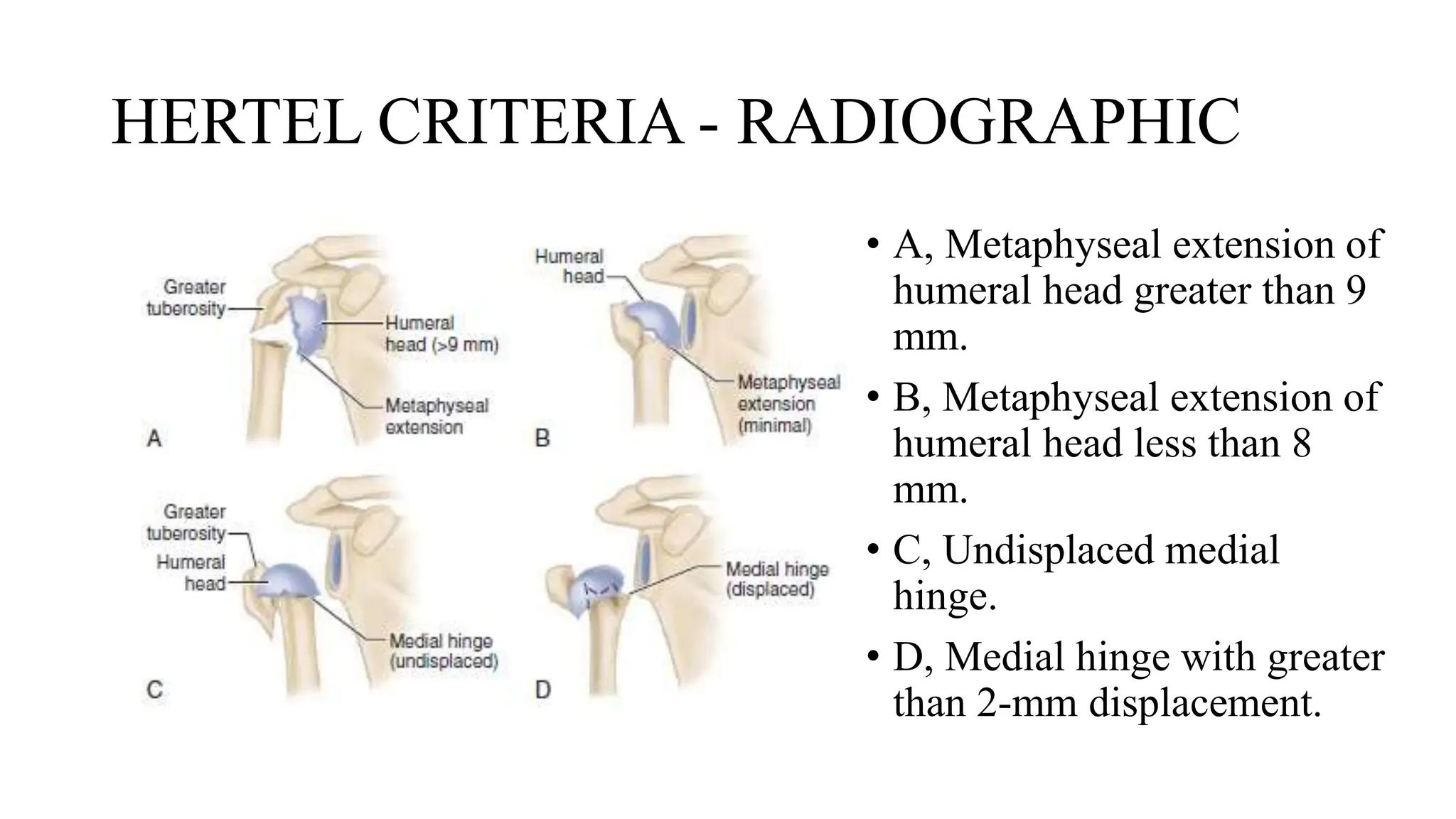
The document discusses the complexities involved in the treatment of proximal humerus fractures, emphasizing the importance of accurate radiographic evaluation and the debate between operative and nonoperative treatment approaches. It notes that while nonoperative treatment may be effective for certain patients, varying success rates and complications warrant careful consideration in treatment decision-making. The text also reviews different surgical techniques, indications for surgery, and the impact of patient factors such as age and bone quality on treatment outcomes.