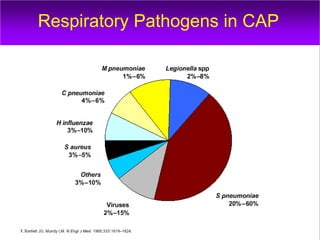
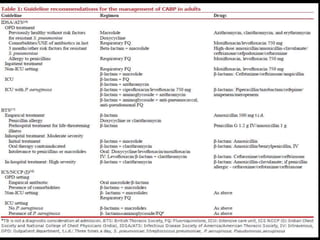
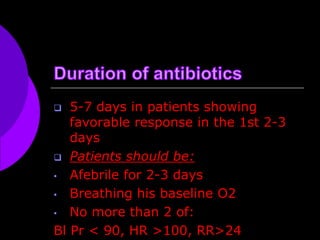
This document discusses community-acquired pneumonia (CAP). It notes that CAP affects 5-6 million people per year in the US, with 20% hospitalized and 10% requiring ICU admission. Mortality rates are 1-5% for outpatients and 12% for inpatients, rising to 50% for those in the ICU. The document reviews common causative respiratory pathogens and risk factors for multi-drug resistant organisms. It also discusses signs and symptoms, diagnostic testing, imaging findings, severity assessment tools, and treatment guidelines for CAP.