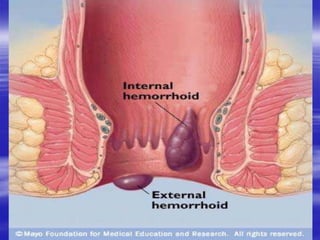
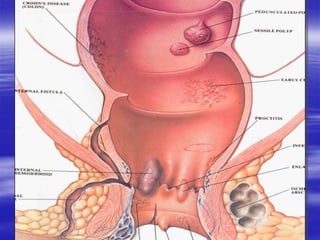
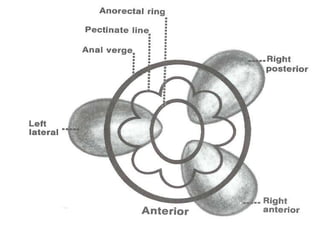
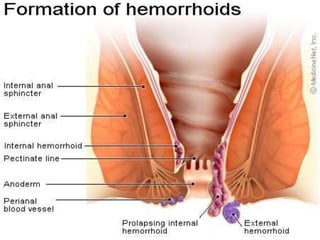
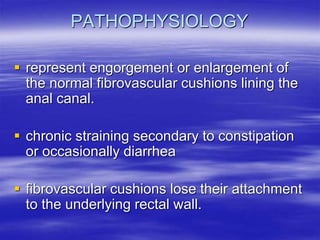
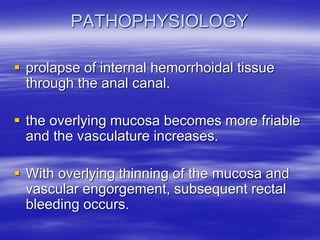
This document discusses hemorrhoids, including their anatomy, classification, pathophysiology, symptoms, physical examination, evaluation, and treatment options. Hemorrhoids are enlarged or swollen veins in the anal canal. They are classified based on their location and degree of prolapse. Common symptoms include rectal bleeding and anal mass or bulge. Treatment ranges from lifestyle and dietary changes to office-based procedures like rubber band ligation or infrared coagulation to surgical hemorrhoidectomy.