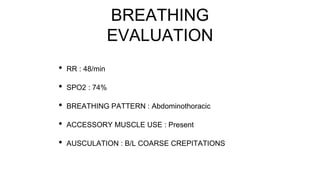
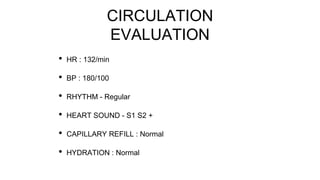
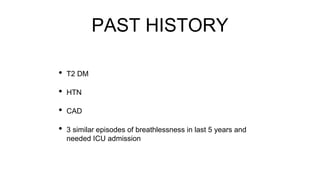
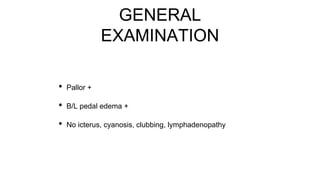
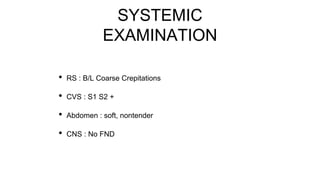
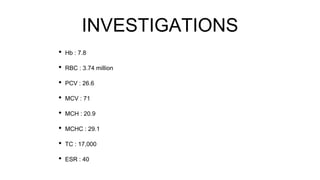
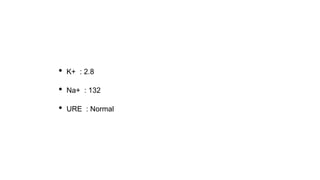
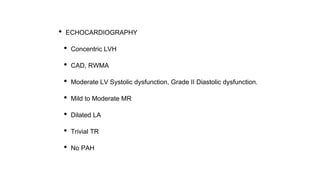
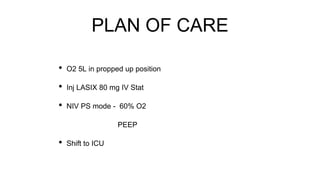
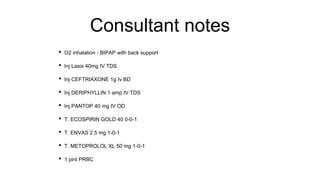
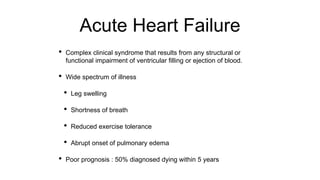
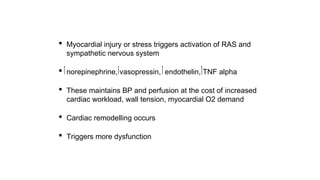
This document presents the case of a 74-year-old male who presented to the emergency department with acute exacerbation of breathlessness, cough with expectoration, and chest pain. On examination, he had tachypnea, hypoxemia, coarse crepitations on lung auscultation, tachycardia, and elevated blood pressure. Investigations revealed anemia and echocardiography showed left ventricular hypertrophy, systolic dysfunction, and diastolic dysfunction. He was diagnosed with acute left heart failure with pulmonary edema and treated with oxygen, diuretics, antibiotics, vasodilators, and transferred to the ICU.