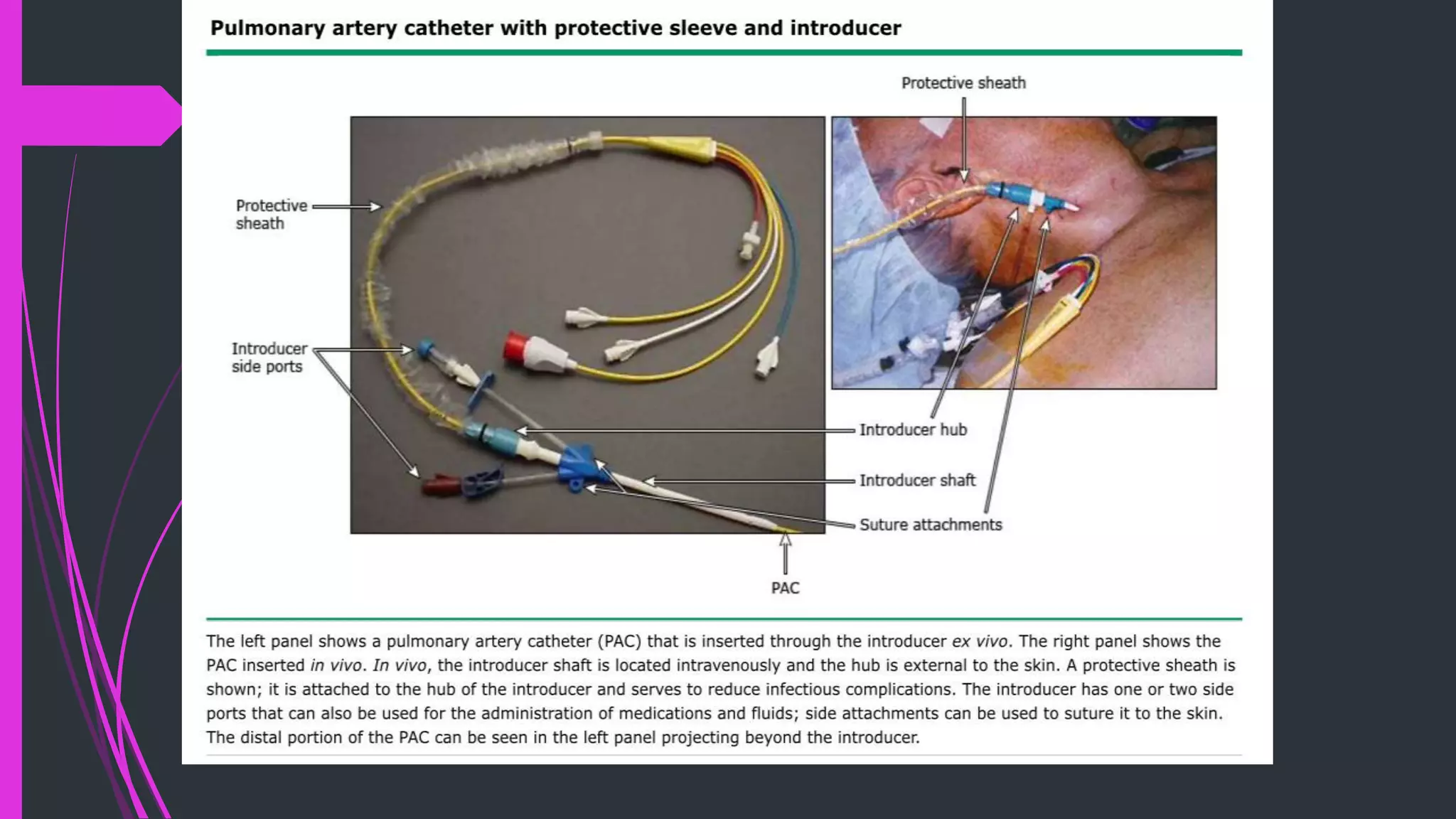
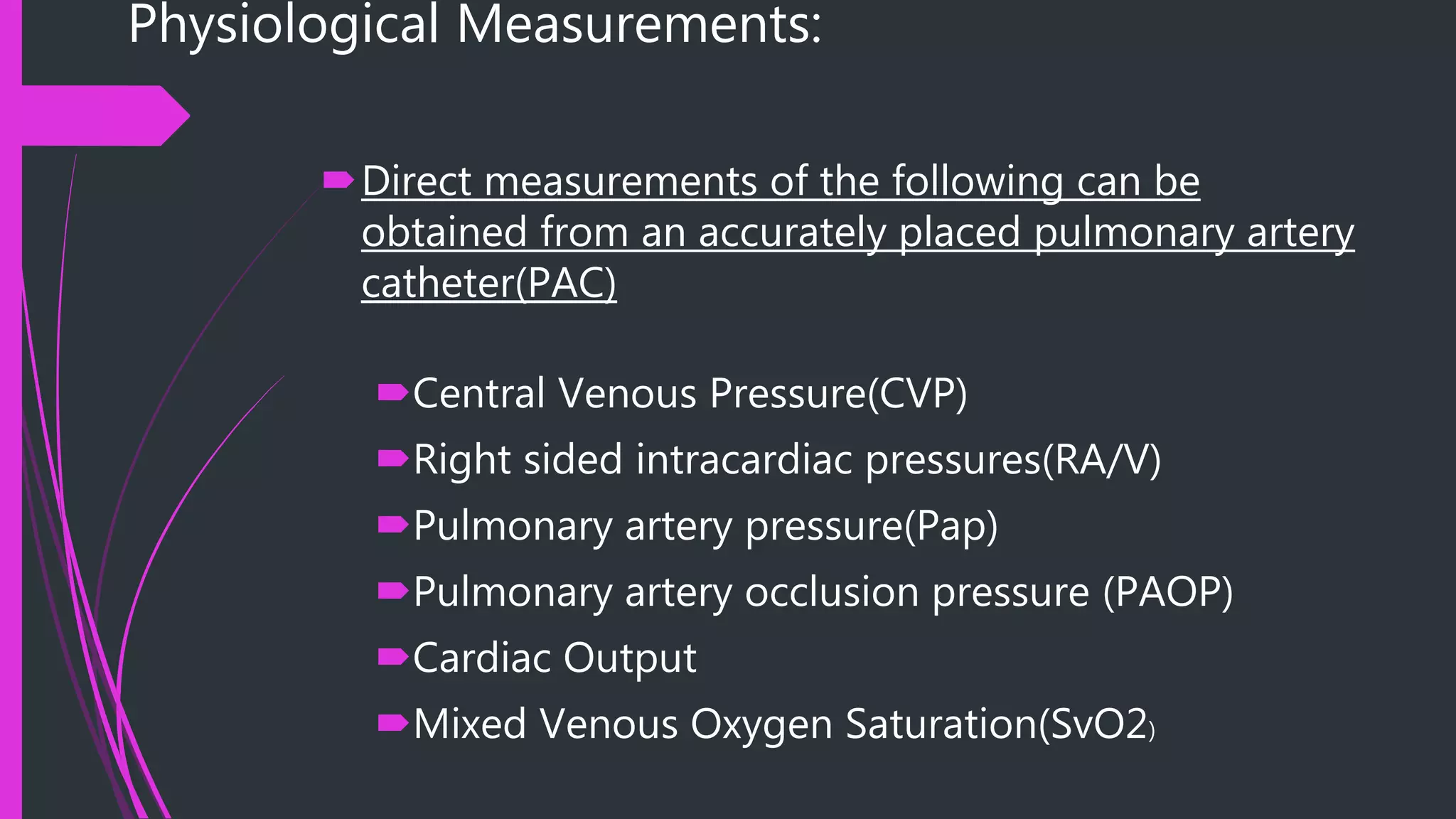
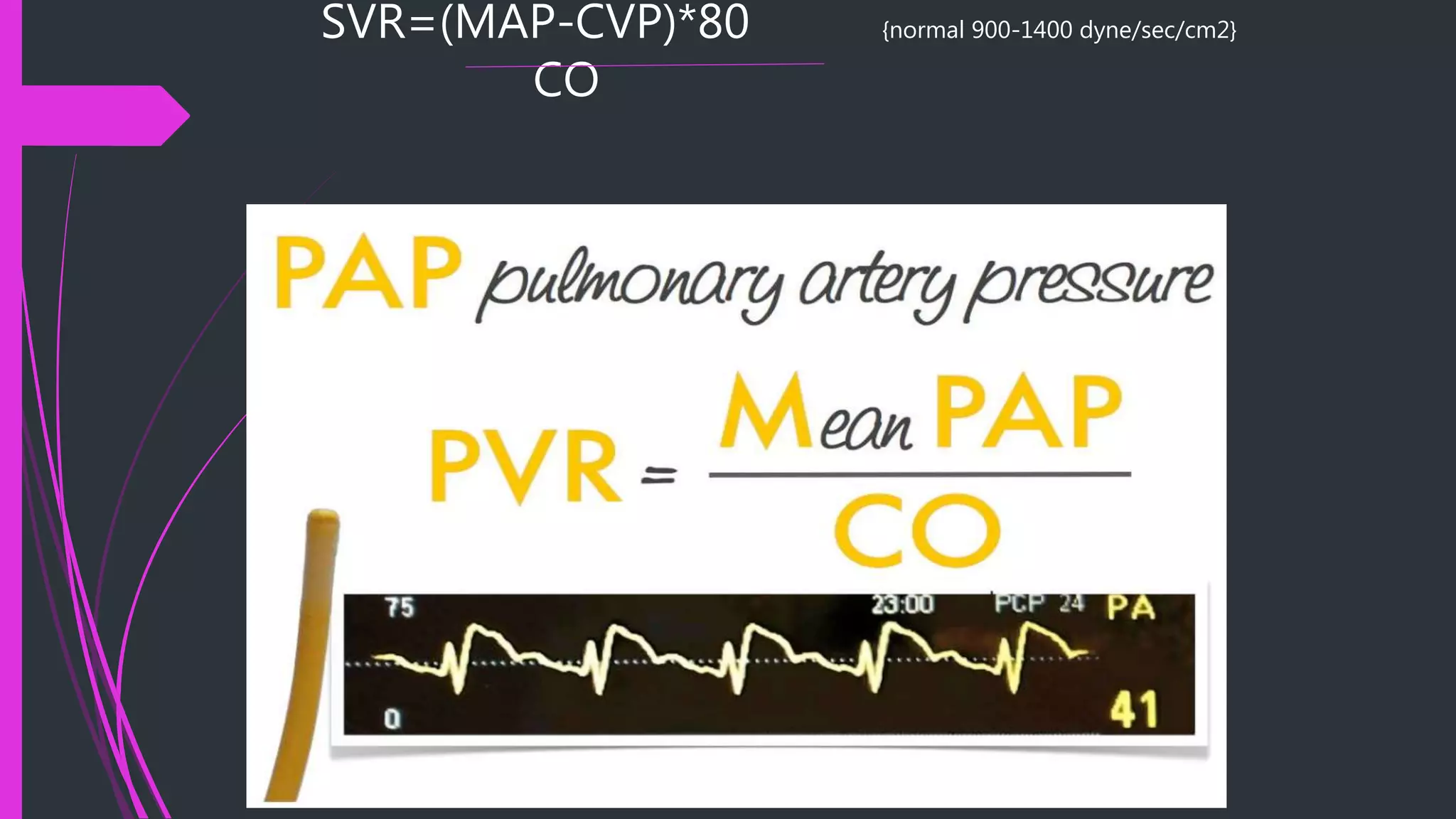
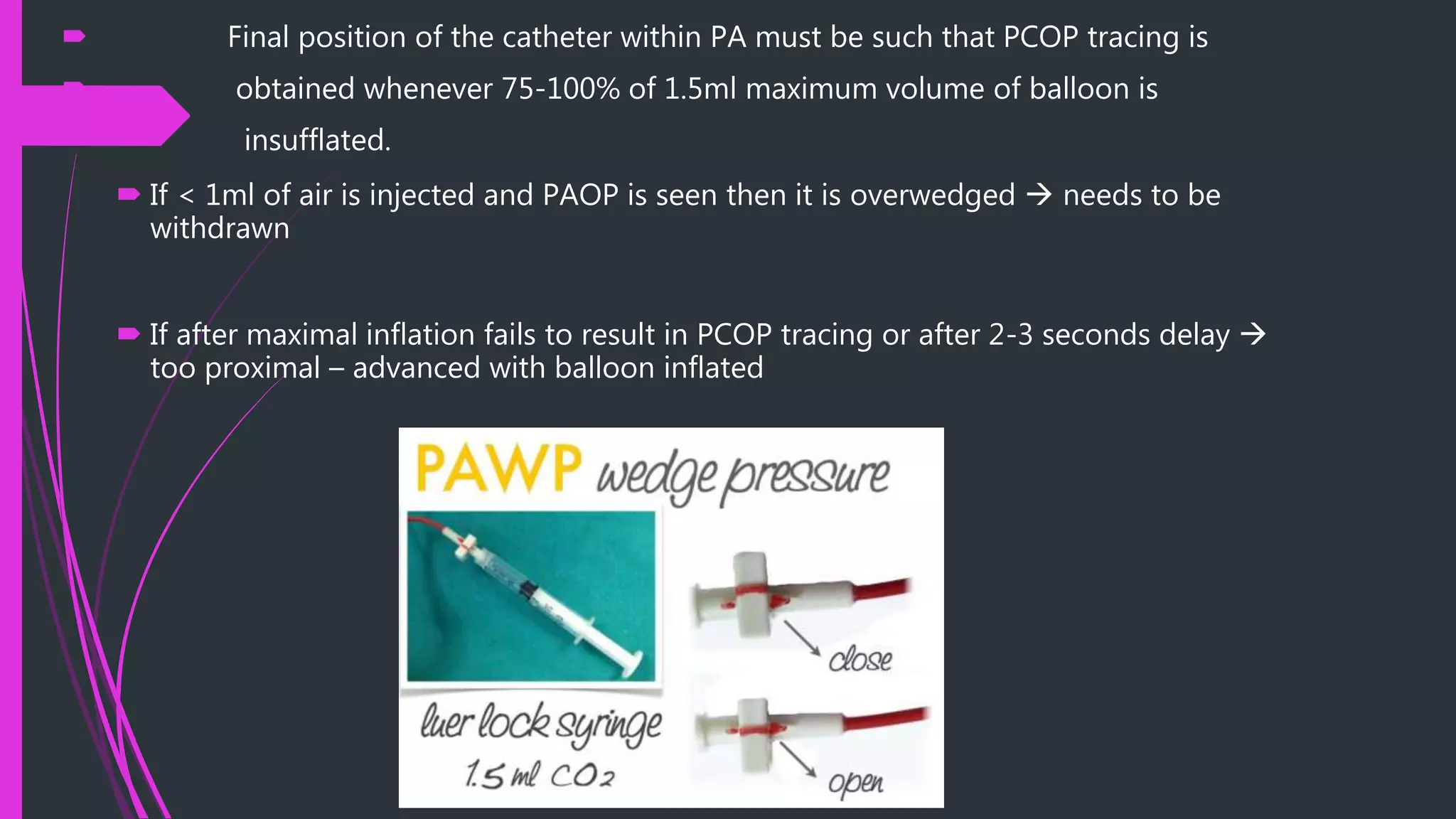
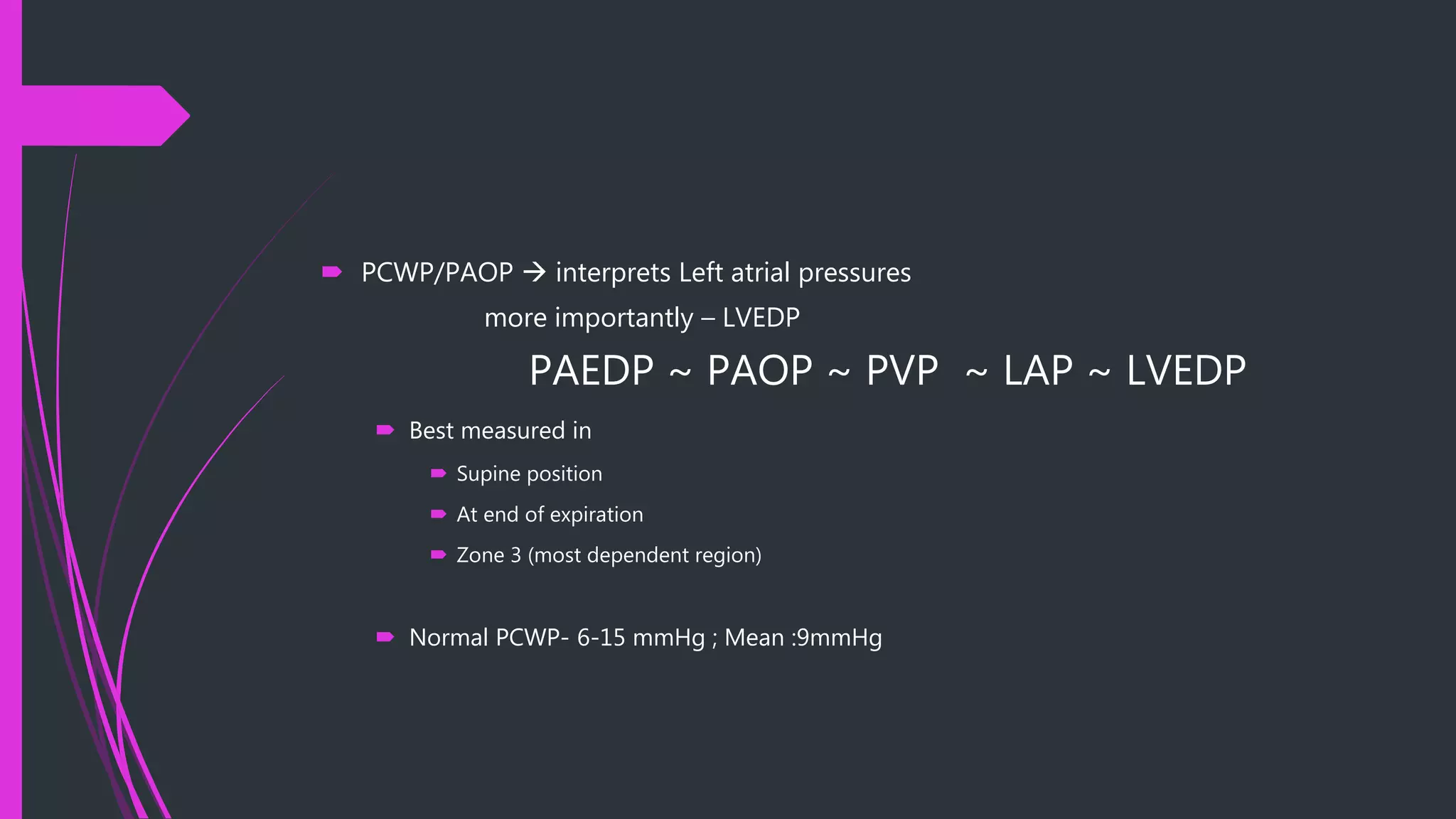
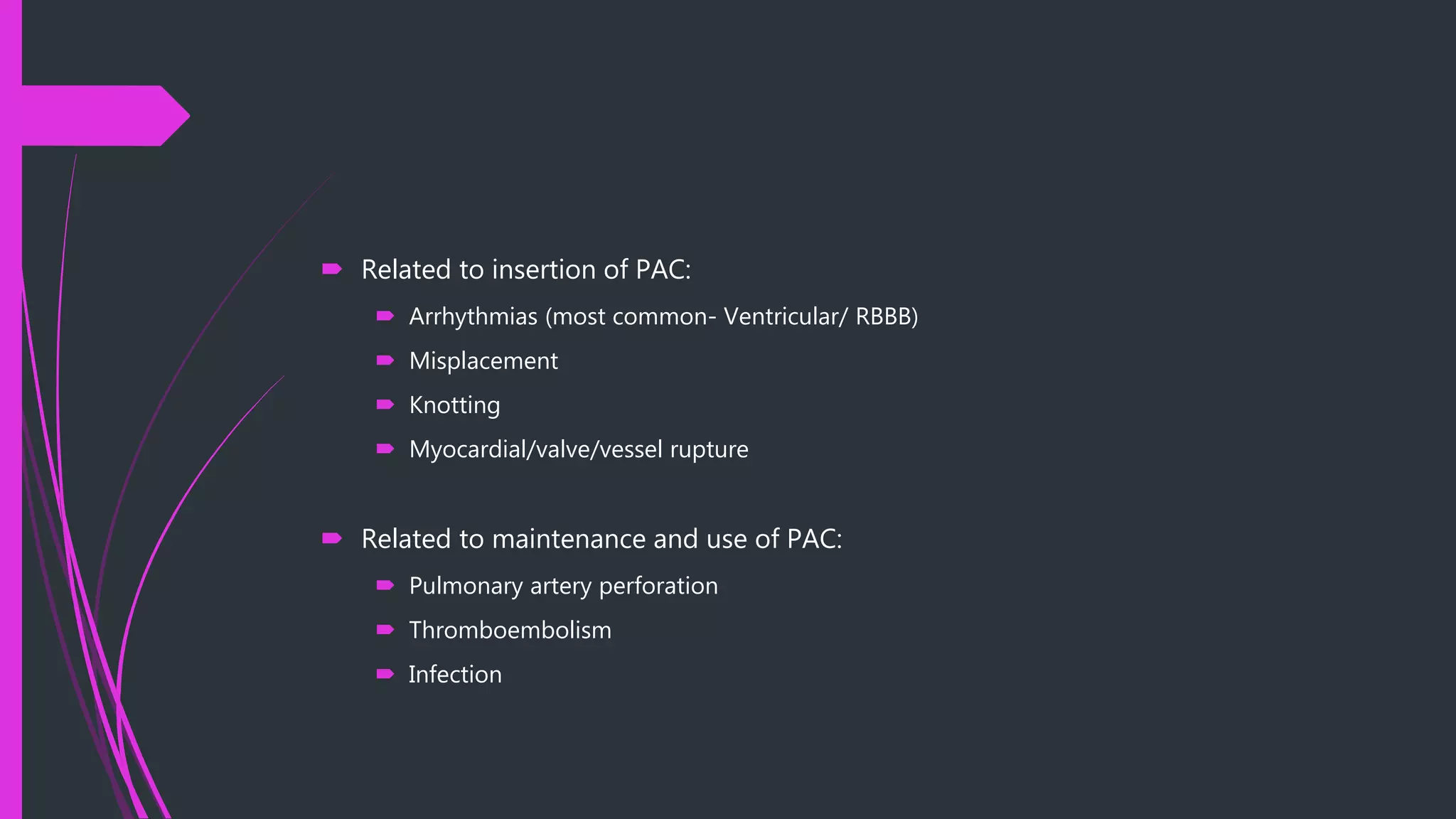
The document discusses the pulmonary artery catheter, including its indications, contraindications, preparation, technique, interpretation of physiological values and waveforms, and complications. The pulmonary artery catheter can be used diagnostically to differentiate causes of shock, types of pulmonary edema, and detect intracardiac shunts. It can also be used therapeutically to help manage high-risk surgery patients, sepsis, heart failure, and guide pharmacologic therapy. Placement involves inserting the catheter into the internal jugular or subclavian vein and advancing it into the pulmonary artery using pressure readings and waveforms as guides. Measurements obtained include pressures, cardiac output, oxygen saturation, and derived values like vascular resistances. Complications include bleeding, arr