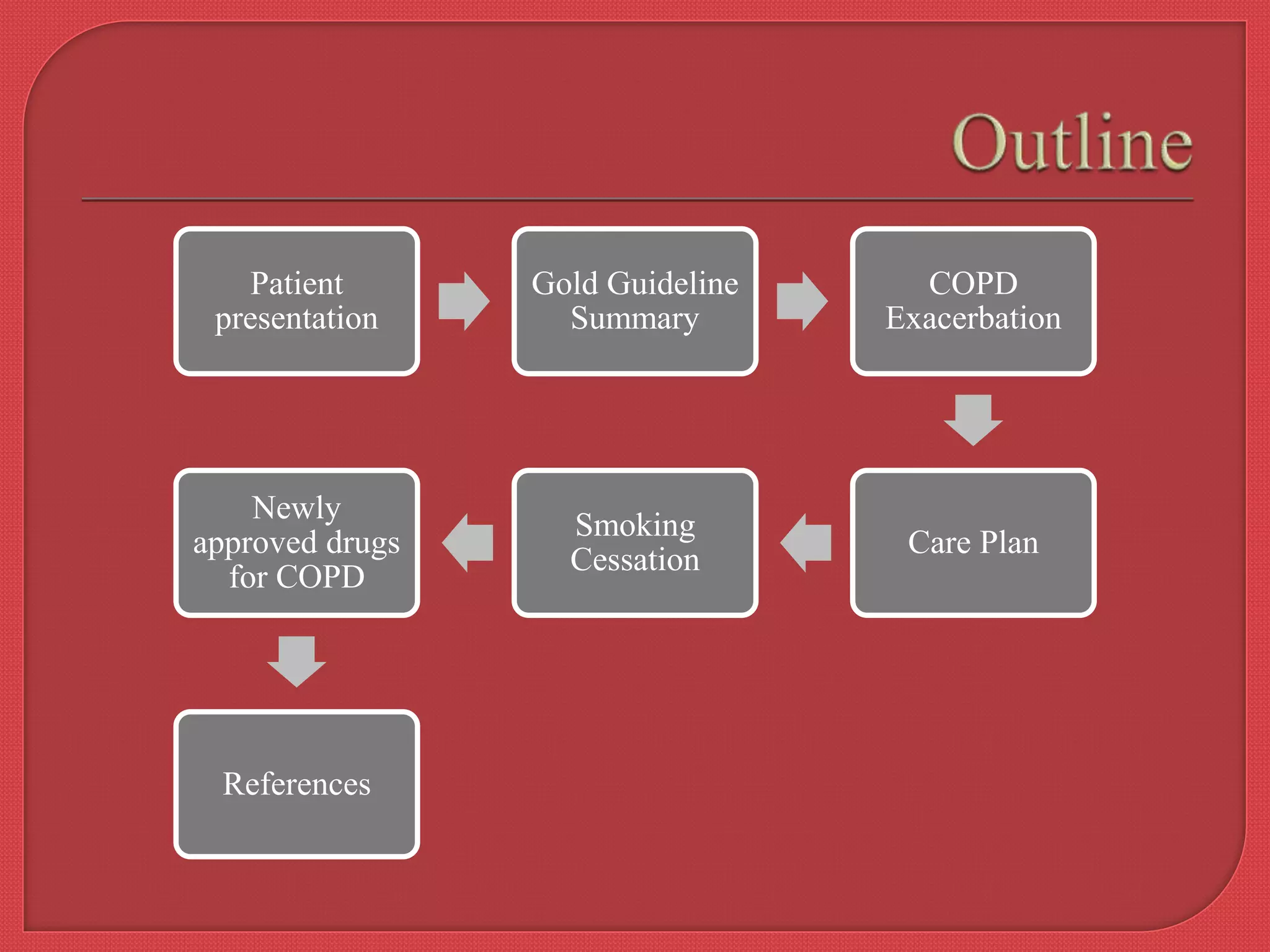
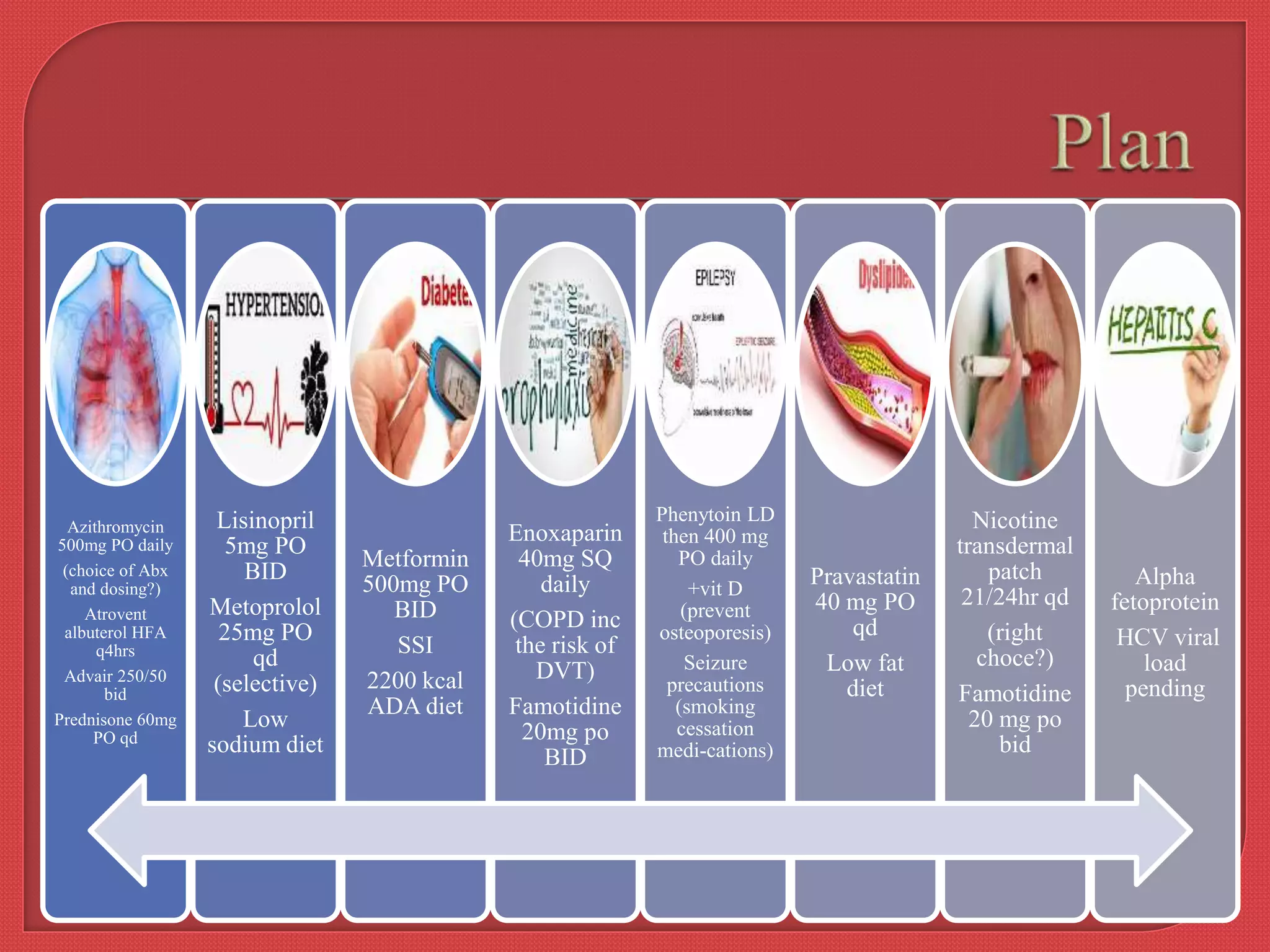
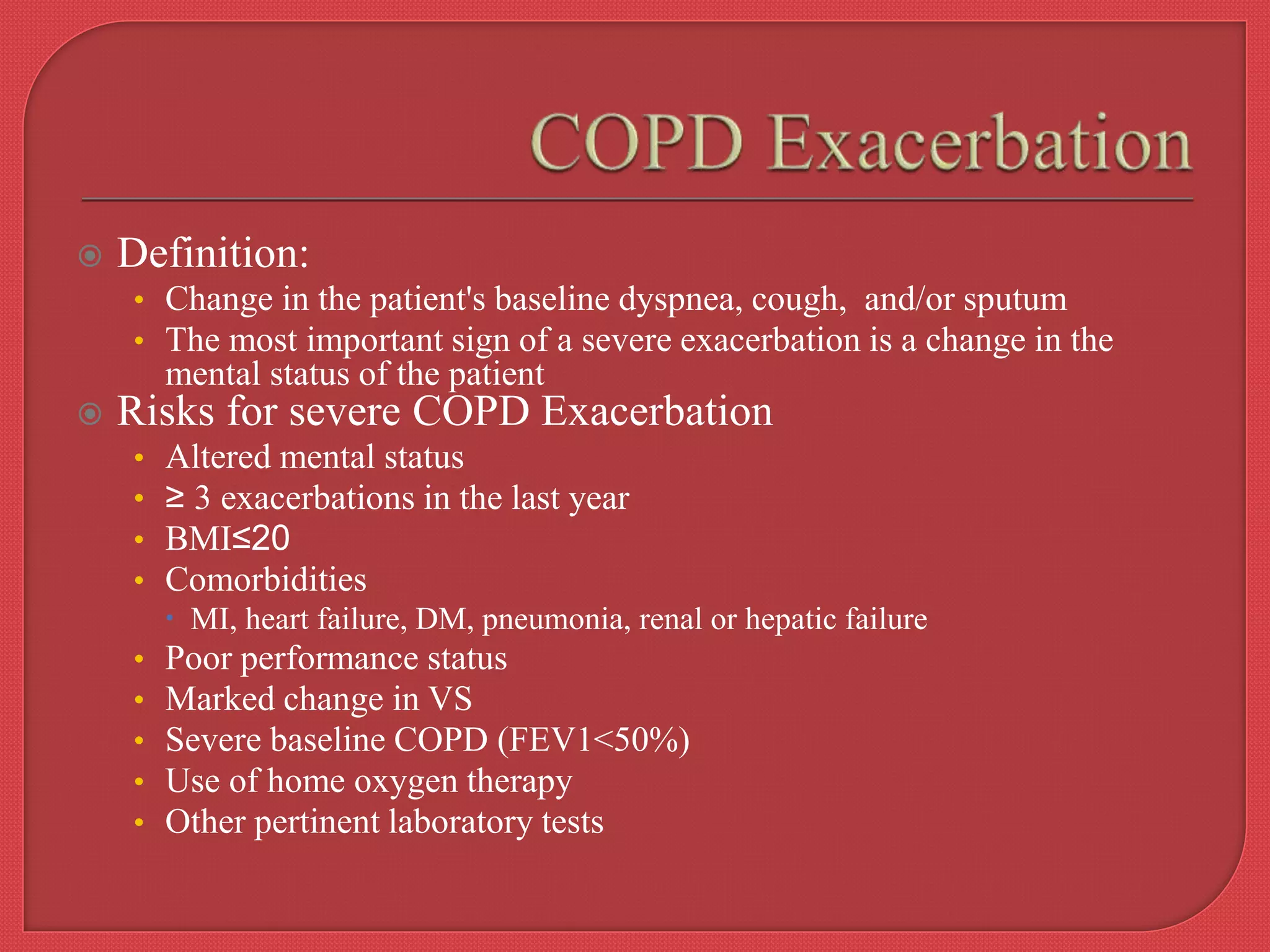
The document presents a detailed case study of a 55-year-old male patient with COPD, highlighting his medical history, current medications, and presenting symptoms. It discusses the management of COPD exacerbation based on established GOLD guidelines and outlines various treatment options, including medications, lifestyle changes, and the importance of exercise therapy. Key points include the need for personalized treatment plans and the role of systemic corticosteroids and bronchodilators in managing exacerbations.