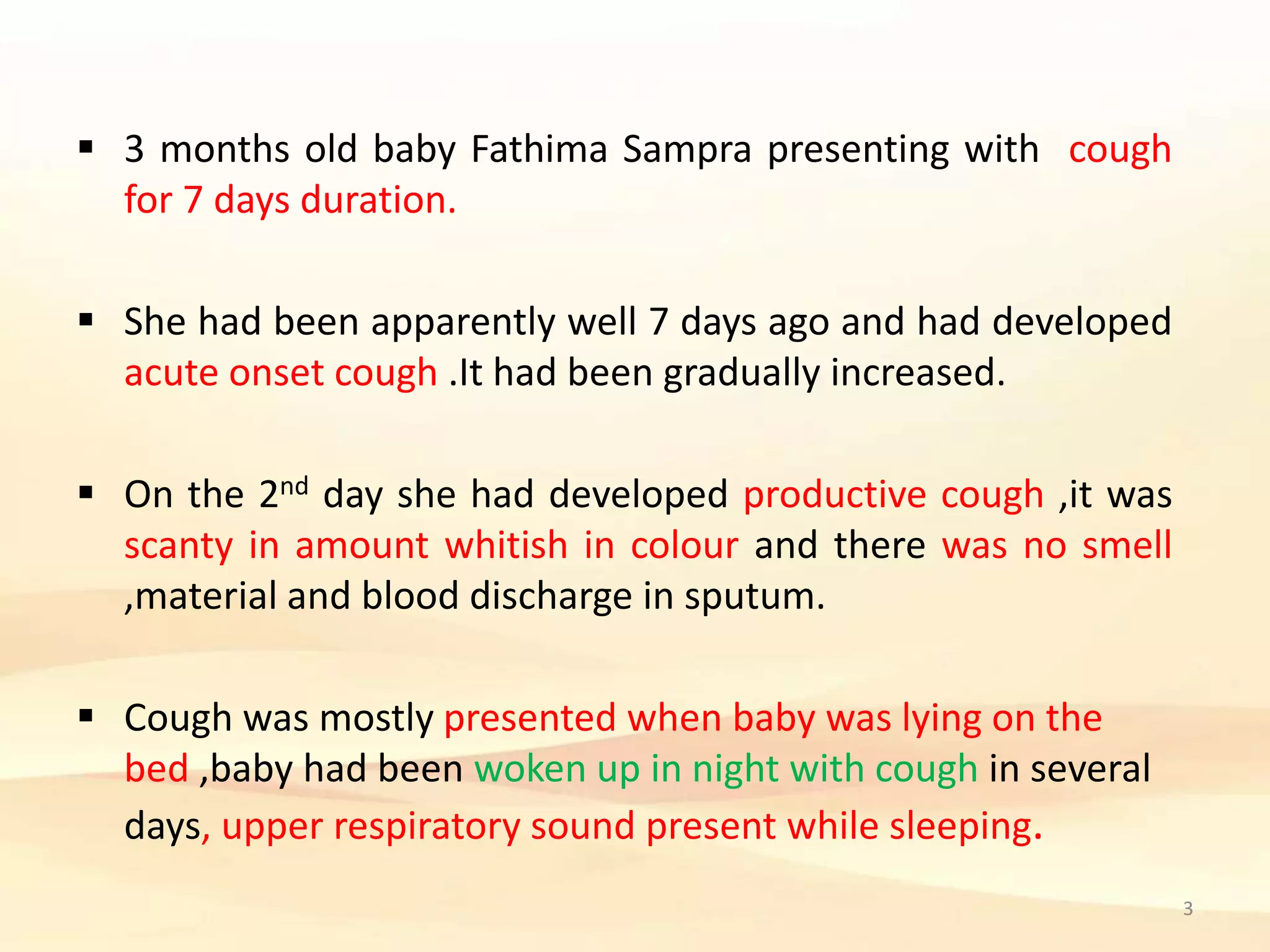
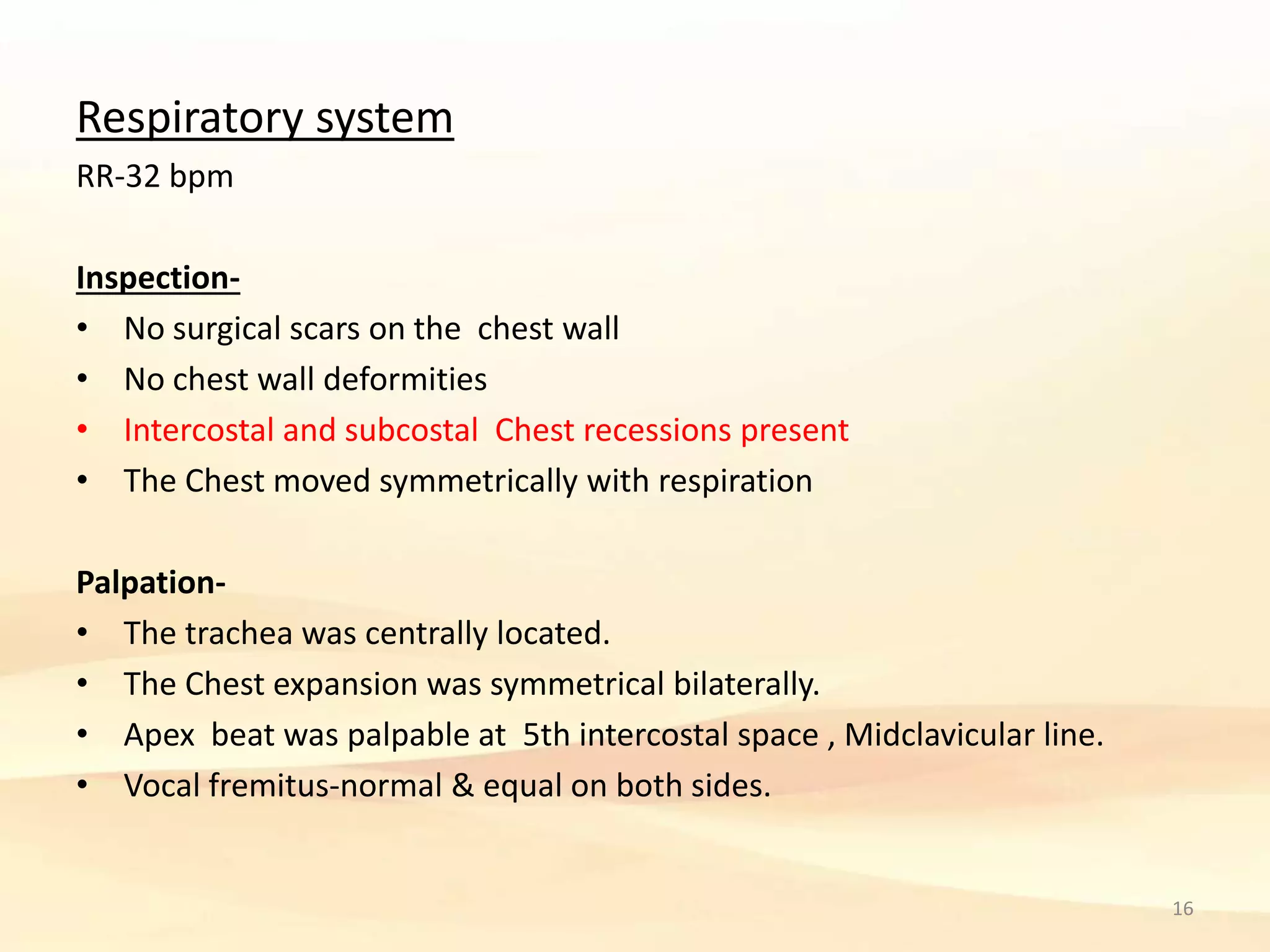
3 month old baby Fathima Sampra presented with cough for 7 days. The cough was worse when lying down and caused waking at night. On examination, the baby had increased respiratory rate and bilateral crepitation at the lung bases. Differential diagnoses included bronchiolitis, bronchial asthma, and pneumonia. Treatment involved nebulized ipratropium and hypertonic saline, along with saline nasal drops. Oxygen supplementation was not needed as the baby's saturation was normal.